The surgical technique of laparoscopic pelvic lymphadenectomy: how to streamline the procedure
Highlight box
Surgical highlights
• We reported a 52-year-old woman with stage IA endometrial carcinoma received a laparoscopic total hysterectomy and pelvic lymphadenectomy (PL).
What is conventional and what is novel/modified?
• PL can be performed using the abdominal approach or laparoscopic approach.
• Our experience in laparoscopic PL for treating patients with endometrial carcinoma was advantageous.
What is the implication, and what should change now?
• PL is an important surgical procedure for gynecological malignancies. A good understanding of basic laparoscopic technique would improve the odds of a successful operation.
Introduction
Pelvic lymphadenectomy (PL) is an important step in the surgical treatment of endometrial cancer. PL can be performed using the laparotomic approach or laparoscopic approach. Several studies have shown that laparoscopic PL (LPL) had lower postoperative complication rates, including less postoperative pain, smaller scar, shorter hospital stay, lower postoperative symptomatic lymphocele, and faster recovery of bowel movement compared to abdominal PL (APL) (1-3). Therefore, LPL is related to better cosmetic result and faster recovery compared to APL. However, the importance of surgical techniques and experience needs to be emphasized. In this case, we reported a 52-year-old woman with stage IA endometrial carcinoma who underwent laparoscopic total hysterectomy and PL. I present this article in accordance with the SUPER reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-15/rc).
Preoperative preparations and requirements
In this case, a 52-year-old female was admitted to the First Affiliated Hospital of Xiamen University due to “irregular vaginal bleeding for 10 days”. Pathological findings of segmented curettage showed poorly differentiated endometrioid adenocarcinoma in this patient. Magnetic resonance imaging (MRI) scan showed a slight thickening of the endometrium and a left chocolate cyst. The diagnosis for this patient was stage IA low differentiated endometrial adenocarcinoma. Therefore, a laparoscopic total hysterectomy with double appendages and PL was performed. There were 15 lymph nodes removed in the left pelvis and 13 lymph nodes removed in the right pelvis. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of the First Affiliated Hospital of Xiamen University (No. 2021GGB027). Written informed consent has been obtained from the patient for the publication of this manuscript and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Step-by-step description
Video 1 provides a step-by-step guide on how to do an LPL.
Step 1
Detailed exploration of the pelvis and abdominal cavity. We sutured the uterus round ligament to suspend the uterus, and performed coagulation of bilateral isthmus of fallopian tubes to avoid tumor cell expansion. We suctioned the peritoneal flushing fluid for cytological examination. During the operation, the left ovary was dissected and a 4-cm chocolate cyst was found and removed.
Step 2
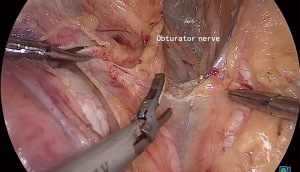
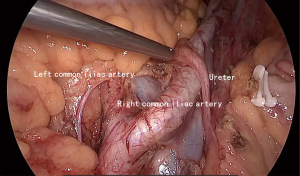
We opened the peritoneum and exposed the boundary of lymphadenectomy. The process of removing lymph nodes requires detailed exposure of blood vessels and nerves. The upper boundary: 2 cm above the common iliac artery (Figure 1). The internal boundary: the internal iliac artery. The bottom boundary: the obturator nerve (Figure 2). The external boundary: the external iliac artery. The lower boundary: the deep iliac circumflex vein. The ureter should be exposed to prevent injury.
Step 3
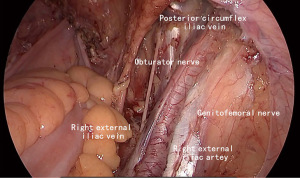
After exposing the lymph node resection boundary, we can resect fat, and lymphatic tissue wrapping blood vessels and nerves (Figure 3), which not only can surgically remove entire lymph nodes but also avoid damage to important blood vessels and organs. We should be careful with the deep iliac circumflex vein, and remove lymph nodes in the triangular region.
Postoperative considerations and tasks
Postoperative pathological findings suggested that endometrial hyperplasia changed, local hyperplasia was disordered, and no residual tumor was found. In addition, all of the lymph nodes were negative.
Early postoperative assessment should be attentive to the following aspects: surgical incision, color, nature, and amount of drainage in the abdominal cavity. Moreover, it is also necessary to pay attention to the changes in the patient’s body temperature. The long-term evaluation included surgical scars, abnormal pain, and pelvic lymphatic cysts.
Tips and pearls
PL requires the removal of fat and lymphatic connective tissue surrounding the large blood vessels and their branches, nerves, and the lateral walls of the pelvis. The resection scope included: the upper boundary reaching 3 cm above the intersection of the internal and external iliac arteries, and the common iliac lymph nodes on the surface of the common iliac artery were removed. The lower boundary was the deep iliac circumflex vein that crosses the external iliac artery, where the surface was a deep inguinal lymph node. The outside boundary reached the junction of the psoas muscle surface and the iliac blood vessels. The inner boundary was the lateral edge of the ureter. The bottom was often marked by the obturator nerve, which could also reach the surface of the pelvic floor muscle beyond the obturator nerve. All lymphatic and adipose tissues within this area should be completely removed, including bilateral common iliac lymph nodes, external iliac lymph nodes, internal iliac lymph nodes, obturator lymph nodes, and deep inguinal lymph nodes.
The basic steps of LPL were the same as those of open PL. First, the surgeon should open the pelvic side wall peritoneum, separate the superficial structure of the pelvic side wall, extend the peritoneal incision down to the round ligament near the inguinal ligament, and extend upward to about 3 cm above the bifurcation of the common iliac artery. At the same time, the peritoneum was medially separated to expose the main trunk of the internal iliac artery. Subsequently, along the loose space between the external iliac blood vessels and the iliopsoas muscle, it was gradually separated to the surface of the obturator muscle, thereby separating the common iliac blood vessels, external iliac blood vessels, obturator nerves, obturator blood vessels, and the surrounding lymphatic adipose tissue from the deep structures such as the pelvic lateral wall muscles and bones. After that, the arterial tunica vaginalis on the surface of the iliac artery was cut open, and the pelvic lymph nodes in each group were excised in a lump from top to bottom or from bottom to top by coagulation. Emphasizing the standardization of surgical procedures can reduce technical errors and complications, improve surgical quality, and shorten the learning curve.
Discussion
PL is an important procedure of surgery for patients with gynecological malignant tumors, and the status of the lymph node is related to the staging, prognosis, and decision-making of postoperative adjuvant treatment (4,5). Extraperitoneal lymphadenectomy has many advantages and is widely used in clinical practice (6). The routes for retroperitoneal lymphadenectomy include open surgery, laparoscopy, and extraperitoneal surgery (7). The location of the trocar placement location varies, depending on the surgical requirements and the personal habits of the surgeon. The most commonly used method is to place the trocar into the endoscope above the umbilicus, with two 5 mm trocars on both sides. Generally, laparoscopic surgery for lymphadenectomy is performed through the abdominal cavity path, which opens the peritoneum from the abdominal side and then removes the subsequent lymph nodes.
The most common parameter used to assess the accuracy of the PM is the number of lymph nodes removed. In this case, 15 lymph nodes were removed from the left pelvis and 13 lymph nodes were removed from the right pelvis. There is no consensus regarding the definition of an adequate lymphadenectomy in gynecologic malignancies among gynecologic oncologists and pathologists. A previous study by Chan et al. demonstrated that the removal of 21 to 25 lymph nodes significantly enhances the likelihood of detecting at least one positive lymph node in endometrial cancer (8). Therefore, the LPL was considered adequate to assess the lymph node status in this case. For patients with lymph node recurrence after surgery, laparoscopic surgery is also a feasible and effective technique (9).
Our experience in the surgical techniques for LPL was as follows: (I) emphasize teamwork: have an excellent assistant to make the surgery faster and safer. (II) Familiarity with anatomy: if the anatomy of blood vessels is not clear during surgery, inaccurate judgment can easily cause vascular damage, and even “devastating” damage to large blood vessels can endanger the patient’s life. (III) Master the anatomical marks and boundaries of PL: lateral boundary—the psoas major muscle, bottom boundary—internal obturator muscle, medial boundary—lateral umbilical ligament, lower boundary—deep iliac circumflex vein. (IV) Key points of surgery: anatomy, sharpness, clearance, and integrity.
Conclusions
In conclusion, PL is an important surgical procedure for gynecological malignancies. A good understanding of basic laparoscopic technique would improve the odds of a successful operation.
Acknowledgments
The video was awarded the third prize in the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery).
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)”. The article has undergone external peer review.
Reporting Checklist: The author has completed the SUPER reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-15/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-15/prf
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-15/coif). The series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of the First Affiliated Hospital of Xiamen University (No. 2021GGB027). Written informed consent has been obtained from the patient for the publication of this manuscript and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hwang JH, Kim BW. The incidence of postoperative symptomatic lymphocele after pelvic lymphadenectomy between abdominal and laparoscopic approach: a systemic review and meta-analysis. Surg Endosc 2022;36:7114-25. [Crossref] [PubMed]
- Uccella S, Laterza R, Ciravolo G, et al. A comparison of urinary complications following total laparoscopic radical hysterectomy and laparoscopic pelvic lymphadenectomy to open abdominal surgery. Gynecol Oncol 2007;107:S147-9. [Crossref] [PubMed]
- Bergstrom J, Aloisi A, Armbruster S, et al. Minimally invasive hysterectomy surgery rates for endometrial cancer performed at National Comprehensive Cancer Network (NCCN) Centers. Gynecol Oncol 2018;148:480-4. [Crossref] [PubMed]
- Bodurtha Smith AJ, Fader AN, Tanner EJ. Sentinel lymph node assessment in endometrial cancer: a systematic review and meta-analysis. Am J Obstet Gynecol 2017;216:459-476.e10. [Crossref] [PubMed]
- Gunderson CC, Java J, Moore KN, et al. The impact of obesity on surgical staging, complications, and survival with uterine cancer: a Gynecologic Oncology Group LAP2 ancillary data study. Gynecol Oncol 2014;133:23-7. [Crossref] [PubMed]
- Richards L. Surgery: Laparoscopy versus laparotomy in early-stage endometrial cancer. Nat Rev Clin Oncol 2010;7:550. [Crossref] [PubMed]
- Scribner DR Jr, Walker JL, Johnson GA, et al. Surgical management of early-stage endometrial cancer in the elderly: is laparoscopy feasible? Gynecol Oncol 2001;83:563-8. [Crossref] [PubMed]
- Chan JK, Urban R, Cheung MK, et al. Lymphadenectomy in endometrioid uterine cancer staging: how many lymph nodes are enough? A study of 11,443 patients. Cancer 2007;109:2454-60. [Crossref] [PubMed]
- Pecorino B, Scibilia G, Sozzi G, et al. Laparoscopic surgery for isolated inguinal node relapse of high grade serous ovarian cancer using a bipolar combination instrument. Surg Oncol 2020;34:283. [Crossref] [PubMed]
Cite this article as: Zhou J. The surgical technique of laparoscopic pelvic lymphadenectomy: how to streamline the procedure. Gynecol Pelvic Med 2024;7:3.