Unruptured ovarian pregnancy: a rare case report
Highlight box
Key findings
• We present an unruptured ovarian pregnancy (OP) and aim to enhance our understanding of the clinical characteristics of OP.
What is known and what is new?
• OP which accounting for 0.5% to 3% of all types of ectopic pregnancy. The onset of OP is acute, severe, and the fatality rate is high. Unruptured OP is extremely rare.
• This case report describes an unruptured OP, we performed the operation in time and avoid the occurrence of malignant events.
What is the implication, and what should change now?
• The rarity of this case adds to the literature understanding the management and treatment of OP.
Introduction
The most common type of ectopic pregnancy (EP) is tubal pregnancy, while EP occurring within ovarian tissue are extremely rare. The incidence of ovarian pregnancy (OP) in women conceiving naturally ranges from 1:2,100 to 1:60,000, accounting for only 0.5–3% of all types of EP (1). Most OP cases result in early pregnancy termination. Due to the thin cortex, decreased elasticity, and rich blood supply of the ovary, most patients are diagnosed with OP after emergency surgery for ruptured bleeding. Preoperative diagnosis of OP is extremely challenging (2). OP with intact ovarian epithelium and an unruptured gestational sac is exceptionally rare.
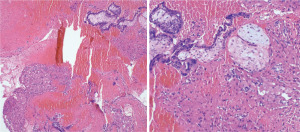
Currently, the diagnostic criteria proposed by Spiegelberg, a gynecologist and obstetrician, in 1878 are still used in clinical practice: (I) both fallopian tubes are intact and separated from the ovaries; (II) the ectopic gestational sac is located within the ovarian tissue; (III) the ovary and gestational sac are connected to the uterus by the ovarian ligament; (IV) histopathological examination confirms the presence of ovarian tissue on the gestational sac wall (3).
OP is a rapidly developing condition characterized by severe symptoms and significant bleeding, posing a life-threatening risk. Its clinical presentation is difficult to distinguish from ruptured tubal pregnancy or ovarian corpus luteum rupture (4). The lack of typical preoperative manifestations makes the definitive diagnosis of OP highly challenging. Therefore, we present a recent clinical case of an unruptured OP in the Second West China Hospital of Sichuan University and aim to enhance our understanding of the clinical characteristics of OP. We present this case in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-29/rc).
Case presentation
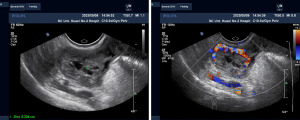
A 22-year-old patient (gravida 1, para 0) presented to the emergency department of the Second West China Hospital of Sichuan University on May 9, 2023, with a chief complaint of “amenorrhea for 48 days, slight vaginal bleeding for 1 day”. The patient has generally been in good health, with regular menstrual cycles in the past. Menarche occurred at the age of 12, with a menstrual cycle length of 3–5 days every 28–33 days. The last menstrual period was on March 22, 2023, with normal menstrual flow and mild dysmenorrhea. After 37 days of amenorrhea, the patient underwent an examination at an external hospital, which revealed a blood human chorionic gonadotropin (HCG) level of 806.1 mIU/mL. The ultrasound conducted at the external hospital showed no gestational sac echo in the uterus, but a weak echo nodule of approximately 13×10 mm was visible in the left ovary. The patient denied experiencing abdominal pain or vaginal bleeding, and no further examinations were performed at that time. After 47 days of amenorrhea, the patient presented with vaginal bleeding that was scant and bright red in color, without abdominal pain, bloating, dizziness, fatigue, or a sense of rectal fullness. Upon admission, the patient’s vital signs were as follows: heart rate 96 beats per minute, blood pressure 115/86 mmHg, respiratory rate 19 breaths per minute. The patient was conscious and cooperative during the physical examination. No abnormalities were found during cardiac and pulmonary examinations. The abdomen appeared normal in shape, was soft on palpation, and showed no tenderness or rebound tenderness. No masses were palpable in the abdomen. During the gynecological examination, the external genitalia were well-developed, the vagina was patent, and a small amount of white discharge mixed with a few red streaks was observed in the vagina. The cervix appeared smooth, with no bleeding on touch, pain on movement, or tenderness. The uterus was retroverted, slightly enlarged, and mildly tender. No masses were palpable in the bilateral adnexal regions, and no tenderness was noted. Transvaginal ultrasound (Figure 1) findings indicated a retroverted uterus with dimensions of 4.6 cm × 5.6 cm × 5.6 cm. The endometrium was centrally located and measured approximately 0.85 cm in thickness (single-layer). No definite gestational sac was visualized within the uterus. On the anterior wall, a weak echo with a diameter of 1.1 cm was observed, with clear boundaries. In the left adnexal region, a slightly heterogeneous echogenic mass measuring 2.5 cm × 1.8 cm × 2.2 cm was detected, with anechoic areas visible within it. The surrounding area of the mass showed a rich blood flow signal in a circular pattern, with a resistive index (RI) of 0.42. Several follicle-like anechoic areas were seemingly present around the periphery of the mass, with a corpus luteum-like echo seen on its deep surface and a semi-circular blood flow signal visible around it. No definite mass was observed in the right adnexal region. A pelvic fluid collection measuring 1.1 cm in depth was identified during the pelvic examination. The serum HCG level was measured at 6,409.8 mIU/mL. No obvious abnormalities existed in blood routine, coagulation function, urine routine and liver and kidney function.
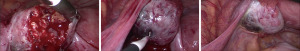
Upon admission, the following diagnoses were considered: (I) vaginal bleeding due to amenorrhea: possible left OP? (II) Uterine fibroids. Preoperative preparations were completed, and a laparoscopic exploration was performed. Intraoperatively (Figure 2), a retroverted uterus was observed, slightly enlarged, with a soft texture. The left fallopian tube showed no signs of thickening or dilation, and the fimbrial end appeared normal without bleeding. There were no adhesions between the fallopian tube and the left ovary. The left ovary showed cystic enlargement of approximately 5 cm × 4.5 cm × 3 cm, adhered to the left pelvic peritoneum. After the adhesions were dissected, the surface of the left ovary appeared smooth, with intact ovarian capsule. Locally, it exhibited a bluish-purple color. Using a unipolar electrocautery, the ovarian cortex was incised along the bluish-purple border, revealing a gestational sac of approximately 2.0 cm with blood clots and trophoblastic tissue inside. The right ovary appeared normal in size and showed no apparent abnormalities. The right fallopian tube also appeared normal. The gestational sac tissue was grasped and removed using a gallbladder forceps, and the surrounding blood clots were carefully cleaned. The ovarian wound was repeatedly irrigated, confirming the absence of residual pregnancy tissue. Finally, the left ovary was sutured using absorbable suture material (2-0, ETHICON, USA) to achieve proper closure. Serum HCG 2,707.3 mIU/mL was reviewed 24 hours after surgery. Postoperative pathology (Figure 3) confirmed OP. Serum HCG <5 mIU/mL 15 days after surgery.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The most common site of occurrence is the fallopian tube, while OP is extremely rare (5). In this case, the patient had complete encapsulation of the pregnancy tissue by ovarian tissue, indicating primary OP. The exact etiology of OP has not been thoroughly studied, but the current etiological factors mainly focus on disturbances in ovum release and fallopian tube motility (6). The ovulation process is complex and requires the synergistic action of reproductive, endocrine and nervous systems. Damage to any of these links can lead to ovulation disorders (6). After pelvic inflammation or adhesion, the ovarian cortex hyperplasia becomes thick, adhesion, and ovulation disorder occurs after the pressure within the follicle is reduced. Inflammation or disease of the fallopian tube leading to tube wall thickening or hydrosalpinx can affect ciliary cell movement, finally prevent ovulation (6). The main high-risk factors for OP include intrauterine device (IUD) use and the use of assisted reproductive technology (ART) (7). Since 1976, IUD has been reported as a high-risk factor for OP, possibly affecting the vitality of the fallopian tube, although the specific mechanism is unclear. Previous literature reported a history of IUD use in 57–90% of patients with OP (8). Recently, Li et al. conducted a retrospective analysis of patients diagnosed with OP from 2005 to 2018 at the West China Second University Hospital of Sichuan University using a case-control study design. They reported that the clinical symptoms of OP were more severe than other types of EP, and the use of IUDs [odds ratio (OR) =2.19] and ART (OR =2.08) were potential high-risk factors (9). Other high-risk factors for OP, similar to tubal pregnancy, include a history of pelvic surgery, adnexal surgery, pelvic inflammatory disease, and endometriosis (10). However, in our case, the patient had no history of IUD use or ART, but intraoperative findings revealed adhesions between the left ovary and the pelvic wall, which may have been the trigger for OP.
The most common clinical manifestations of EP are “amenorrhea, abdominal pain, and vaginal bleeding”, and the clinical presentation of ruptured OP is similar to that of tubal pregnancy. Specific and typical symptoms of OP have not been reported in literature (10). In this case, the patient did not complain of abdominal pain but only presented with minor vaginal bleeding for one day. Similar to the diagnosis of tubal pregnancy, the definitive diagnosis of OP requires a comprehensive assessment of detailed medical history, physical examination, transvaginal ultrasound, serum beta-HCG levels, and their dynamic changes. Radiological examinations such as magnetic resonance imaging (MRI) or computed tomography (CT) may be necessary, and the final diagnosis requires intraoperative findings and postoperative pathology.
The doubling of blood HCG levels in patients with EP is usually poor, often failing to double within 24 hours. However, the value and doubling pattern of HCG have low specificity and sensitivity in diagnosing OP. In this case, the patient had a 47-day menstrual delay, with a serum HCG level of 6,409.8 mIU/mL. Transvaginal ultrasound revealed no definite gestational sac in the uterus, but a mass was found near the left adnexa, which led us to preliminarily consider a higher possibility of EP. Preoperative examination time is limited, and ultrasound examination is convenient, time-saving, and can be performed at the bedside, making it an indispensable auxiliary diagnostic tool. In the diagnosis of EP, transvaginal ultrasound has significantly higher specificity than transabdominal ultrasound (6). Foreign studies have proposed common B-mode ultrasound characteristics of OP: (I) a wide echogenic ring on the ovarian surface with an echogenic area inside; (II) presence of ovarian cortical signals and the presence of corpus luteum or follicles around the mass; (III) echogenicity of the ring is greater than that of the ovary itself (11). In this case, transvaginal ultrasound showed follicle or corpus luteum-like echoes around the mass. After repeated communication with the ultrasound specialist, it was unanimously considered that there was a higher possibility of OP. After sufficient communication with the patient and family members, laparoscopic exploration was performed, and the intraoperative findings and pathological examination were consistent with the diagnostic criteria for OP, thus avoiding the occurrence of severe complications.
Laparoscopic minimally invasive surgery is considered the preferred treatment for OP. The surgical approach aims to “remove the ectopic pregnancy lesion and preserve the normal ovarian tissue to the greatest extent possible” (2). Partial wedge resection of the ovary is recommended, and the use of energy devices should be avoided during the procedure. Methotrexate is the most commonly used for EP. Methotrexate causes destruction of the trophoblast and embryo, leading to the formation of blood clots within the ovary, which increases the size of the lesion and reduces the presence of muscular tissue around the ovary, thereby increasing the risk of ovarian rupture and intra-abdominal hemorrhage (1). In this case, in order to minimize the impact on ovarian function, we used suture closure for hemostasis. It is important to note that surgery does not guarantee complete removal of pregnancy tissue, and trophoblastic tissue infiltrating the ovarian cortex may not be completely cleared. Postoperatively, closely monitoring of serum HCG levels and symptoms is necessary, and if necessary, drug therapy or repeat surgery may be required.
Conclusions
OP has a low incidence, and non-ruptured OP is even rarer. Currently, ultrasound has become the primary diagnostic tool for OP. Laparoscopic surgery is considered the optimal treatment for OP due to its minimally invasive nature, minimal trauma, and shorter hospital stay. The frequency of OP is on the rise, making its diagnosis and management crucial. There have been no reports of ovarian function decline after an OP surgery, but as gynecologists we need to strike a balance between removing pregnancy tissue and preserving normal ovarian tissue.
Acknowledgments
We would like to extend our greatest thanks to this female patient for trusting her care with us and allowing us to share her story.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-29/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-29/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-29/coif). X.N. serves as an unpaid Executive Editor-in-Chief of Gynecology and Pelvic Medicine. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zoukar O, Zouari I, Jemaa Y, et al. Ovarian pregnancy case study and literature review. Pan Afr Med J 2021;40:208. [PubMed]
- Bouab M, Touimi AB, Jalal M, et al. Diagnosis and management of ectopic ovarian pregnancy: a rare case report. Int J Surg Case Rep 2022;91:106742. [Crossref] [PubMed]
- Spiegelberg O. Zur Casuistik der Ovarialschwangerschaft. Archiv für Gynäkologie 1878;13:73-9. [Crossref]
- Ren F, Liu G, Wang T, et al. Unruptured ovarian ectopic pregnancy: Two case reports and literature review. Front Physiol 2022;13:1036365. [Crossref] [PubMed]
- Almahloul Z, Amro B, Nagshabandi Z, et al. Ovarian Pregnancy: 2 Case Reports and a Systematic Review. J Clin Med 2023;12:1138. [Crossref] [PubMed]
- Stewart LM, Stewart CJR, Spilsbury K, et al. Association between pelvic inflammatory disease, infertility, ectopic pregnancy and the development of ovarian serous borderline tumor, mucinous borderline tumor and low-grade serous carcinoma. Gynecol Oncol 2020;156:611-5. [Crossref] [PubMed]
- Joseph RJ, Irvine LM. Ovarian ectopic pregnancy: aetiology, diagnosis, and challenges in surgical management. J Obstet Gynaecol 2012;32:472-4. [Crossref] [PubMed]
- Aleem FA, Kim ES. Primary ovarian pregnancy and the intrauterine contraceptive device. Arch Pathol Lab Med 1981;105:112-4. [PubMed]
- Li H, Liu Y, Yang Y, et al. Clinical analysis of women with ovarian pregnancy: a retrospective case-control study. BMC Pregnancy Childbirth 2022;22:768. [Crossref] [PubMed]
- Zhu Q, Li C, Zhao WH, et al. Risk factors and clinical features of ovarian pregnancy: a case-control study. BMJ Open 2014;4:e006447. [Crossref] [PubMed]
- Levine D. Ectopic pregnancy. Radiology 2007;245:385-97. [Crossref] [PubMed]
Cite this article as: Luo C, Niu X, Chen Y, Mei L. Unruptured ovarian pregnancy: a rare case report. Gynecol Pelvic Med 2023;6:35.