Adverse events in women with neglected vaginal pessaries for pelvic organ prolapse: a case report and literature review
Highlight box
Key findings
• Pessaries rarely cause serious adverse effects of urethra, rectum and reproductive system, such as urinary retention, pessary impaction, urogenital fistula, malignant tumor. The occurrence of rare complications about vaginal pessaries is almost entirely related to long-term wearing and improper care.
What is known and what is new?
• The vaginal pessary is a simple, economical, safe and effective conservative treatment for symptomatic pelvic organ prolapse.
• This is the first case to list all cases of pessary impaction and cancers related to pessary
What is the implication, and what should change now?
• Gynecologists and caregivers should inform pessary users in detail about the standard care of the pessary and the necessity of regular follow-up in order to avoid the occurrence of adverse events.
• Future studies are needed to determine consensus recommendations of follow-up and complication management, and to develop patient-specific pessaries for different individuals to improve patients’ satisfaction with pessary use.
Introduction
Background
Pelvic organ prolapse (POP) is defined as pelvic organ displacement and decline caused by the defect or relaxation of pelvic floor supporting tissue, which has become one of the global public health problems affecting women’s health and quality of life (1). There are generally no symptoms in the early stage of POP, patients will have varying degrees of lumbosacral discomfort, vaginal irregular bleeding, urination disorders, sexual dysfunction, vulva infection, etc., in the middle and late stages. The vaginal pessary is a device that supports the uterine and vaginal walls and keeps them in the vagina, which can restore the pelvic organs to their anatomical position. It is a simple, economical, safe and effective conservative treatment for symptomatic POP. The conservative therapy is used especially in the case of elderly frail women, medical complications that hinder surgery, women with fertility requirements or during pregnancy, patients unwilling to undergo surgery, those seeking symptom relief while awaiting surgery and POP patients with stress urinary incontinence (2). There are two types of pessaries: support type and space-filling type at present (3). Supporting pessary is placed in the posterior vaginal fornix to prevent POP by supporting the pubic bone or pelvic floor and are currently the most widely used type in clinical practice. Ring pessary is the most commonly used supporting pessary due to its easy removal and replacement without affecting sexual life, and is commonly used for mild to moderate uterine prolapse. The space-filling pessary is generally larger in volume and is the first choice when the supporting pessary is not effective. The removal of this type of pessary is more difficult than that of ring pessary, and it is necessary to remove the pessary in the vaginal intercourse. A Gellhorn is a commonly used space-filling pessary for moderate to severe uterine prolapse or vaginal anterior and posterior wall prolapse (4).
Rationale and knowledge gap
The most common complications of wearing a pessary are unpleasant odor, vaginal discharge, bleeding, pain, and constipation. If POP patients are willing and able to remove, clean and replace the pessary themselves, complications can be effectively avoided. Pessaries rarely cause serious adverse effects of urethra, rectum and reproductive system, such as urinary retention, pessary impaction, urogenital fistula, malignant tumor, etc. (5). The occurrence of these rare complications is almost entirely related to long-term wearing and improper care. At present, there is no uniform standard for the follow-up and management of pessaries after wearing, which is largely based on the opinions of experts and the specific situation of patients. However, the importance of regular assessment must be stressed to all wearers, even if they feel comfortable or asymptomatic while wearing the pessary. At the beginning of wearing the pessary, patient satisfaction should be assessed after 1 to 2 weeks of wearing the pessary, and follow-up should be conducted every 3 months for the first year of wearing the pessary and every 6 months thereafter.
Objective
The aim of this study was to report three rare cases of neglected pessaries developing impaction, cervical intraepithelial neoplasm (CIN) and endometrial cancer finally and to summarize incarcerated vaginal pessaries and malignant tumors of the genital tract related to neglected pessaries, in order to emphasize the importance of use and care of the vaginal pessary. We present these cases in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-25/rc).
Case presentation
Case 1
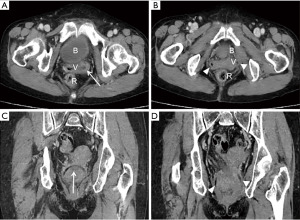
A 77-year-old vaginally grand multiparous woman who had been wearing a pessary for POP for more than 40 years presented with management of worsening vaginal pain. She had not regularly replaced and cleaned the pessary in the past 40 years. Three years prior to presentation, this patient developed vaginal pain, increased viscous leucorrhea, bloody vaginal secretions, and has been taking antibiotics intermittently until now. This patient’s surgical history included open cholecystectomy and open bowel resection and anastomosis were performed because of intestinal perforation after intestinal polypectomy. There was no evidence of any other essential disease. Vaginal examination revealed a ring-shaped pessary was obliquely incarcerated in the middle and lower parts of the vagina, part of the front edge of the pessary was visible at the vaginal orifice, and the rest was embedded in the vagina walls (Figure 1). Rectal examination showed no abnormalities. The pelvic floor ultrasound showed that part of the pessary echo in the cervix of the upper part of vagina was semi-circular, and part of it seemed to be embedded in the cervical wall. A computed tomography (CT) scan showed a ring-like low-density image in the vagina, standing up and down, spreads the left and right-side walls of the vagina, and the width of the middle of the vaginal cavity is about 6 cm without invasion of the bladder and rectum (Figure 2). Under general anesthesia, vaginal examination revealed an incarcerated ring pessary. The visible portion of the ring pessary was grasped and divided completely by cutting it into 4 pieces with a scalpel and the pessary was removed by sliding it through the epithelial tunnel out of the vagina (Figure 3). The pessary is about 5 cm in diameter. She was discharged on the next day and offered conjugated estrogen cream. She had no symptoms of POP and did not complain about vaginal discharge and other symptoms with 6 months of follow-up.
Case 2
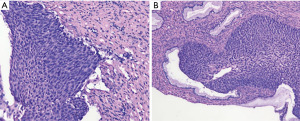
A 69-year-old post-menopausal G4P4 Chinese woman originally presented with vaginal mass prolapse for more than 40 years. After all spontaneous deliveries, the patient consciously started to feel a mass out of the vaginal orifice, complaining of the mass increased after walking and increasing abdominal pressure, and it was completely reducible when lying on the bed. She had no symptoms of urinary incontinence, urinary irritation and constipation. Then she was referred to local hospital with a tubaeforme vaginal pessary (Figure 4) placement 40 years ago and not examined periodically. Before coming to our hospital, she was admitted to another institution for vulvar pruritus, the tubaeforme vaginal pessary had been removed and the cervical cytology indicated atypical squamous cells of unknown significance (ASC-US), further cervical biopsy showed that grade II–III cervical intraepithelial neoplasia (CIN II–III). She denied the history of hypertension, diabetes and heart disease. On vaginal examination, it was revealed that there was POP stage III [POP quantification (POP-Q): Aa +1, Ba +2, C −2, gh 4.5, pb 2, TVL 8, Ap +1.5, Bp +1.5, D −4] after pessary removal and an erosion surface with a size of about 1 cm × 1 cm can be seen on the posterior lip of the cervix. After a biopsy consultation in our hospital, she was diagnosed with CIN III. The patient underwent cervical conization, then she was performed the laparoscopic total hysterectomy, bilateral adnexectomy, Le Fort operation and perineosynthesis under the general anesthesia, after the intraoperative frozen pathological section showed no carcinoma. Postoperative pathological results revealed that CIN III (Figure 5). Vaginal ultrasound and cervical cancer screening showed no significant abnormalities during the six-month follow-up period.
Case 3
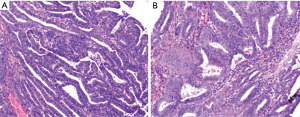
A 63-year-old Chinese woman was referred to our gynecology clinic with a 1-year history of postmenopausal vaginal bleeding. She had a clinical history for wearing vaginal pessary 5 years ago for symptomatic POP; however, she had not seen any gynecologist since then. She took out the pessary on her own before coming to our hospital. Vaginal ultrasound at our institution showed a strong echo approximately 3.5 cm × 2.4 cm × 3.8 cm in the uterus cavity, the boundary with muscle wall partially was not clear, and abundant blood flow signal was detected, which suspected endometrial cancer, so we did not further evaluate the stage of POP. Venous ultrasound of both lower extremities detected right calf intermuscular vein thrombosis. A CT scan showed did not show any characteristic of metastasis but a small amount of mural thrombus formation in the abdominal aorta and its branches. There is no surgical contraindication after consultation by vascular surgeon. She received low molecular weight heparin (LMWH) anticoagulant therapy for three days and stopped medication 24 hours before surgery. Intraoperative pathologic result from endometrial biopsy reported atypical endometrial hyperplasia with focal carcinoma. Then she underwent hysterectomy with bilateral salpingo-oophorectomy and bilateral pelvic and para-aortic lymph node dissection. Pathological findings revealed that highly moderately differentiated endometrioid adenocarcinoma, International Federation of Gynecology and Obstetrics (FIGO) stage IB (Figure 6). This patient had been receiving LMWH anticoagulant therapy since surgery, but still developed pulmonary embolism on the 6th day after surgery. Fortunately, she was successfully discharged on the 10th day and it is recommended to continue taking rivaroxaban orally for at least 3 months. The patient was advised to undergo vaginal brachytherapy (VBT) or continue follow-up. The patient chose to continue follow-up and the test results at 3, 6 and 9 months after operation showed that tumor markers [cancer antigen (CA)125 and CA19-9] was within the normal range and vaginal ultrasound indicates no mass in the pelvic cavity. We will continue to follow-up this patient.
All procedures performed in this study were in accordance with the ethical standards of hospital Ethics Committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
POP is one of the common diseases of pelvic floor dysfunction, which occurs in up to 50% of parous women (6). Depending on the clinical symptoms and therapeutic purposes of POP, pessaries are mainly used to relieve prolapse symptoms, treat stress urinary incontinence, and improve intestinal symptoms and sexual function (3). They are made of medical-grade silicone, which has the merit of making the devices inert and less likely to produce odors or cause allergic reactions (6). Researches show that 87% to 98% of clinicians report using pessaries in their clinical practice, while 77% of gynecologists regarding pessaries as one of the first-line treatment for POP (3,4). Two-thirds of women may choose a pessary as an initial management of their POP, most women who report successful pessary use at 4 weeks continue to use a pessary at 5 years (7,8). The ring support pessaries mainly apply to POP-Q stage I and II prolapse, while the space-occupying pessary is suitable for POP-Q stage III and IV prolapse and can be an alternative option when a ring pessary fails to keep in place or to alleviate prolapse (6). Optimal follow-up and management strategies of vaginal pessaries have no uniform standard, typically based on expert opinion and specific condition of patient. The patient should be seen again within 2 to 4 weeks to evaluate satisfaction including comfort, pessary contention, convenience, and relief of symptoms after well-fitting (6). It may be necessary to change the shape or size of the pessary to prevent it from being falling off by the Valsalva maneuver or movement. Providers should recommend that women who are able to self-care to remove the pessary every week to month and clean it with soapy water or water alone depending on their preference, and to undergo an office follow-up visit at least every 6 months. Women who cannot take care of themselves should initially be followed up every 3 months in the first year and 6-month intervals thereafter (6). The occurrence of adverse effects is almost entirely related to long-term wearing and improper care. Common complications of pessaries include vaginal bleeding, discharge, erosions, pain, discomfort and infection. Complications rates vary from report to report. Bai et al. (9) reported a high complication rate of 73%, but more than 70% of women felt satisfied with the pessary and were reluctant to remove it, therefore indicating that these complications are not severe. These findings contrast with those of a study by Hanson et al. (10), who reported a low complication rate of 11%. Although the pessary is a relatively safe and effective treatment option for POP, serious adverse events still can occur such as urinary retention, pessary impaction, urogenital fistula, malignant tumor (5). Among them, 91% involved pessaries that had been neglected (6). Like the three pessary patients in our article, none of them had regular follow-up after wearing the pessary and adherence to treatment by health professionals. They came to our hospital with adverse events of pain, itching and bleeding respectively due to neglected pessary. We searched the PubMed and GeenMedical databases using the keywords “pessary”, “incarceration”, “neglected”, “impaction”, “entrapment”, and “case”, and found 20 case reports including 23 cases of incarcerated pessary in the English literature between 1977 and 2021, the median age was 76.5 years (51–91 years) accounting for the present case 1 (Table 1). Ring and Gellhorn were the most common pessary types among these studies, 20 (83.3%) and 3 (12.5%) patients, respectively. Among these cases, nearly 67% of these cases (16 of the 24 cases) found occurred between 3 and 40 years of neglected pessary, whereas only 4 cases happened rapid incarceration of ring pessary. The cause of rapid incarceration may be the presence of vaginal ulcers before insertion of the vaginal pessary and their healing occurred around the pessary (13). When vaginal pessaries remain unchanged for prolonged periods, chronic stimulation caused by the neglected pessary can lead to ulcers and re-epithelialization, which may be the reason for the vaginal pessary being clamped and difficulty in removal (2). Andrikopoulou et al. (25) described an unusual case of an elderly frail woman with multiple potential medical issues, manifested by an overlooked impacted pessary, resulting in occult vaginal bleeding and a large vaginal hematoma. Besides, Table 2 summarizes the information including malignant tumors of the genital tract associated with pessary use in available literature, the median age was 75 years (55–98 years). A few studies indicate that pessary use may be a causal mechanism for both vaginal and cervical cancers (32,35). CIN is the precancerous stage for cervical cancer, often occurs in women between the ages 25–35. The concurrence of cervical cancer with POP is rare, partly due to their significantly different age distribution. Cervical cancers tend to occur at about 50 years old and become younger in average age whereas POP typically occurs in an older population of women 1–2 decades beyond the peak incidence of cervical cancers (36). Although the second patient in our case not diagnosed with cervical cancer, but if the patient did not pay attention to the symptoms of genital pruritus, the outcome may be different. Schraub et al. (35) reported a case series of 96 pessary users over 20 years at two institutions, in which 68 cases of cervical cancer and 28 cases of vaginal cancer were associated with pessary use. Since almost all tumors occurred at the site of pessary insertion, the authors concluded that chronic inflammation of foreign bodies associated with viral infection was the likely cause of cancers. Although, primary vaginal carcinoma is not common (accounting for 1–2% of gynecological malignancies), Jain et al. (32) reported that of 9 cases of vaginal cancer reported between 2003 and 2005, 2 cases of vaginal cancer occurred in patients using shelf pessaries. The exact mechanism of carcinogenesis is not known now, probably because neglected pessaries can lead to metaplasia and dysplasia of squamous mucosa. Interestingly, Dawkins et al. reported the first case of cervical cancer complicating POP using a pessary to restore anatomy for optimal radiation (36). Vanichtantikul et al. (37) reported a case of an old woman with multiple medical conditions presenting with POP stage IV combined with endometrioid adenocarcinoma was treated with radiotherapy and pessary placement. To our knowledge, the third patient was the first case to develop abnormal bleeding and endometrial cancer with a neglected pessary. Though it is not clear whether the endometrial cancer was associated with the neglected pessary, we should highlight the importance of close follow-up and periodic assessment for patients with vaginal pessaries to prevent aforementioned adverse events. All patients need to undergo cervical cancer prevention screening and endometrial ultrasound examination before placing vaginal pessary to exclude cervical and endometrial lesions. Vaginal ulcers and vaginitis should be treated before wearing a pessary. In menopausal women with estrogen deprivation, vaginal Lactobacillus species decrease and pH level increase can result in dysregulation of vaginal microenvironment or vaginitis (38). Otherwise, vaginal atrophy in menopause leading to dryness, dyspareunia, discomfort, and pruritus (39). Long-term pessary use may develop erosions of the vaginal mucosa, thereby exacerbating the above changes which can be reversed with local estrogen therapy. Based on expert opinion, topical estrogen therapy is recommended in conjunction with pessary use to prevent or treat vaginal erosions (38). We need to inspect the vaginal mucosa carefully and allow any areas of ulceration to heal with the help of local estrogen cream which soften the fibrotic tissue and make the vagina more supple prior to insertion of a pessary. With patience and the application of local estrogen cream, the incarcerated pessaries can also be easily removed. For the effect of estrogen on vaginal complications of pessary use, the latest meta-analysis provided an answer that local estrogen in combination with a pessary could decrease the bacterial vaginosis rate among postmenopausal women with POP but there is no consensus on decreasing other pessary complications. Additional multicenter randomized controlled trials with large sample sizes should be conducted to better understand the effects of local estrogen use on reducing pessary-related complications (40). The indications and contraindications of wearing pessary should be strictly controlled. There are almost no absolute contraindications of vaginal pessaries, the patients with senile dementia, cognitive impairment and mental disease are not under control need specially-assigned person to care, we should weigh the pros and cons before making a decision otherwise. In order to optimize the safe use of pessaries, providers must be aware of the risks and benefits associated with pessaries, be vigilant during the necessary follow-up, and be prepared to appropriately refer women with pessary related problems beyond their scope of practice (5). Regular follow-up at scheduled visits is important to prevent adverse events in women with neglected vaginal pessaries through early interventions, such as refitting for pessary size and shape, temporary or permanent pessary removal, treatment of any active infection, and/or modifying the vaginal environment with acidifying products or vaginal estrogen (5). The findings of this study have to be seen in light of some limitations: Firstly, these patients wore the pessary for different lengths of time, so it is not clear how long it would take to develop complications. Therefore, the importance of self-care and regular follow-up must be emphasized. Secondly, the sample size of this paper was too small and this review is based on the author’s own analysis and summary of the existing literature which were mainly case reports, prospective randomized and controlled design researches are needed to conducted in the future.
Table 1
| Case | Author, year | Age, years | POP stage | Pessary type; size | Duration of pessary use | Examination | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | Thornton, 1977, (11) | 59 | NA | Ring pessary; 95 mm | 4 months | Gross ulceration of both anterior and posterior vaginal walls. Two areas of the anterior wall had fused over the pessary totally trapping it in the vagina | Local treatment with acriflavine packs and Savlon baths; perform a vaginal hysterectomy and repair operation |
| 2 | Poma, 1981, (12) | 87 | NA | Ring pessary; NA | NA | The pessary was mobilized due to adhesions and stenosis of the outer third of the vagina; the levator muscles contraction | Conjugated estrogen cream; the pessary was removed |
| 3 | Poma, 1981, (12) | 79 | NA | Gellhorn pessary; stem, 6 cm, diameter 7.5 cm | 8 years | Changes in vulvar and vaginal atrophy and contraction of the levator muscles around the bottom of the disc prevent pessary movement, and adhesions prevented rotation around the stem | Conjugated estrogen cream; the pessary was removed |
| 4 | Poma, 1981, (12) | 74 | NA | Gellhorn pessary; NA | 10 years | NA | The pessary was removed |
| 5 | Whitworth, 2002, (13) | 73 | Cystocoele and rectocoele with uterine descent POP-Q stage II | Ring pessary; 80 mm | 5 months | The ring pessary was distinctly visible but cannot be removed with simple traction. Further examination showed a 2–3 cm bridge of vaginal mucosa, originating from the posterior vaginal wall and covering a portion of the ring | Remove the pessary by resecting a portion of it and then rotating the pessary until the excised portion was under the bridge of tissue |
| 6 | Chou, 2003, (14) | 82 | NA | Ring pessary; NA | >10 years | One third of the ring pessary was deeply embedded in the vaginal vault | The pessary was removed |
| 7 | Liang, 2004, (15) | 70 | NA | Ring pessary; 80 mm | >3 years | The ring-shaped pessary was embedded in the vaginal wall | The pessary was cut into two pieces and successfully removed |
| 8 | Ka Yu, 2004, (16) | 51 | NA | Three ring pessaries (54 mm/68 mm/74 mm) | 2 months | After removing those two ring pessaries, it was found that the cervix was enveloped by the innermost ring pessary | The pessary was cut and removed |
| 9 | Nallendran, 2006, (17) | 86 | Uterovaginal prolapse with cystocele and rectocele POP-Q stage III | Ring pessary; 80 mm | 10 years | The pessary was incarcerated in a band of vaginal tissue in the posterior vaginal wall | Removing the pessary by cutting out the band of vaginal tissue; vaginal hysterectomy with pelvic floor repair |
| 10 | Govind, 2007, (18) | 75 | Moderate cystourethrocele | Ring pessary; 80 mm | 4 months | The pessary was embedded in the vaginal wall with a 3 cm band of tissue entrapping it | The pessary was severed by a bone cutter and passed through the epithelised tunnel being released |
| 11 | Fernando, 2007, (2) | 76 | NA | Ring pessary; NA | 4 years | The ring pessary was found to be embedded into the vaginal epithelium, forming a bridge on the pessary | An orthopedic bone cutter is used to grasp the visible part of the ring pessary and completely separate it, sliding the pessary out of the vagina through an epithelial tunnel |
| 12 | Fernando, 2007, (2) | 77 | NA | Ring pessary; NA | 32 years | An incarcerated metal ring pessary | The metal ring with its fragmented latex covering was removed by digital separation from the vaginal skin |
| 13 | Sankar, 2008, (19) | 79 | NA | Ring pessary; 54 mm | Not reported | The pessary was bound by hard fibrous tissue which had greatly narrowed the vagina opening | The pessary was separated using an orthopedic bone cutter and easily removed in two parts |
| 14 | Berger, 2009, (20) | 81 | NA | NA | 28 years | The pessary was found to be half visible, protruding through a midline skin defect under the introitus and one more posterior and lateral | Using an orthopedic “heavy cutter”, the visible part of the pessary was removed, after which the perineal part was rotated out of the perineum |
| 15 | Dasari, 2012, (21) | 60 | NA | Metal ring | 30 years | A metallic aluminum bangle with a diameter of 10 cm was found to be embedded in the vagina with dense fibrosis | One course of broad-spectrum antibiotics, doxycycline and metronidazole for 10 days; The vaginal fibrosis covering the ring was gently cauterized with a 40-watt unipolar cauterization then the ring was removed |
| 16 | Thubert, 2014, (22) | 84 | NA | Ring pessary; NA | 5 years | Her vagina was protruding from her body, trapped within a ring pessary | Removal of the pessary requires a cold knife excision device; a new doughnut-shaped pessary was successfully installed in place |
| 17 | Manivasakan, 2013, (23) | 55 | NA | Ring pessary; NA | 3 years | The posterior semicircle of the pessary was incarcerated in the posterior vaginal wall and the 2 cm vaginal epithelium band covered the ring | Under intravenous sedation, the vaginal bridge was incised with a scalpel, the incision was stanched with catgut ligation, and the pessary was removed |
| 18 | Jain, 2014, (24) | 72 | Uterovaginal prolapse POP-Q stage II | Ring pessary; NA | 12 years | A ring pessary was buried in vagina, with band of tissue overgrowing the ring of the fornix on both sides | The band of vaginal tissue needs to be cut and divided by the removal of the pessary under a short period of general anesthesia |
| 19 | Andrikopoulou, 2015, (25) | 91 | NA | Gellhorn pessary; NA | 14 years | An impacted Gellhorn pessary in the vagina was noted with some spotting | Pessary removal under general anesthesia |
| 20 | Abdool, 2015, (26) | 64 | Cystocele POP-Q stage II | Ring pessary; 70 mm | NA | A thick band of granulation tissue (approximately 2 cm) had grown over the pessary | Local anesthetic was injected into the granulation tissue and the pessary was incised and removed |
| 21 | Cabral Ribeiro, 2017, (27) | 87 | NA | Ring pessary; NA | NA | A pessary intimately adhering to the vaginal wall with an intense inflammatory reaction | Removal of pessary |
| 22 | Ghanbari, 2019, (28) | 84 | NA | Ring pessary; NA | 10 years | An entrapped ring pessary in severely atrophic vaginal mucosa with purulent discharge | After 10 days of treatment with vaginal estrogen and antibiotic (oral metronidazole 500 mg twice a day), the impacted pessary was removed from fibrotic vaginal bundles under spinal analgesia |
| 23 | Pereira, 2021, (29) | 72 | Genital prolapse POP-Q stage IV | Ring pessary | 3 years | The anterior vaginal mucosa involved and wraps the posterior semicircle of the pessary, covering part of its 2-cm epithelium band | She underwent a mucosal incision and a pessary removal under local anesthetic |
| 24 | Present case | 77 | NA | Ring pessary | >40 years | A ring-shaped pessary was obliquely incarcerated in the middle and lower parts of the vagina, part of the front edge of the pessary was visible at the vaginal orifice, and the rest was embedded in the vagina walls | The visible portion of the ring pessary was grasped and divided completely by cutting it into 4 pieces with a scalpel and the pessary was removed by sliding it through the epithelial tunnel out of the vagina |
POP, pelvic organ prolapse; NA, not available; POP-Q, POP quantification.
Table 2
| Case | Author, year | Age, years | Cancer type, stage | Pessary type; size | POP stage | Duration of pessary use | Vaginal examination | Treatment | Follow up |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Russell, 1961, (30) | 55 | Vaginal cancer | Ring pessary; NA | NA | 9 years | A crescent-shaped primary vaginal cancer involving the posterior fornix and the right wall of the vagina | NA | NA |
| 2 | Russell, 1961, (30) | 66 | Vaginal cancer | Ring pessary; NA | NA | 10 years | An ulcerating carcinoma of the vagina involving the posterior fornix and the right upper half of the right vaginal wall | NA | NA |
| 3 | Russell, 1961, (30) | 74 | Vaginal cancer | Ring pessary; NA | NA | Over 40 years | A horseshoe-shaped cancer of the vagina involving the anterior and both lateral walls | NA | NA |
| 4 | Russell, 1961, (30) | 84 | Vaginal cancer | Ring pessary; NA | NA | 10 years | An extensive cancer of the vagina involving the posterior fornix and extending round both lateral walls almost as far as the urethra | NA | NA |
| 5 | Russell, 1961, (30) | 75 | Vaginal cancer | Ring pessary; NA | NA | 20 years | A crescent-shaped cancer involving the posterior fornix and right vaginal wall | NA | NA |
| 6 | Russell, 1961, (30) | 77 | Vaginal cancer | Ring pessary; NA | NA | 50 years | A crescentic cancer of the upper vagina involving the fornix and both lateral walls | NA | NA |
| 7 | Martin, 2013, (31) | 72 | Vaginal cancer, II | Gellhorn pessary; NA | NA | 7 years | A necrotic mass measured approximately 4 cm × 6 cm × 3 cm on the right vaginal wall, apex, and rectovaginal septal area was noted | Vaginal brachytherapy | NA |
| 8 | Jain, 2016, (32) | 96 | Vaginal cancer | Shelf pessary; NA | NA | Several years | A nodule of about 1 cm in diameter was noted on the right lateral wall of the vagina | No | Died within a few months due to other medical problems |
| 9 | Jain, 2016, (32) | 88 | Vaginal cancer | Shelf pessary; NA | NA | Over 7 years | An induration over the posterior vaginal wall with contact bleeding was noted | No | Died a few months later |
| 10 | Akino, 2016, (33) | 60 | Vaginal cancer, IVb | Ring pessary; NA | III | Over 11 years | A 4-cm vaginal tumor became apparent at the right vaginal wall | Chemotherapy using paclitaxel (175 mg/m2) and carboplatin (AUC =6) was administered | Live and lung metastases, died of disease after two courses of chemotherapy |
| 11 | Tan, 2021, (34) | 81 | Vaginal cancer | Ring pessary; 80 mm | IV | 4 years | There was a vaginal wall ulcer in the posterior fornix measuring 3 cm × 3 cm | Vaginal hysterectomy and bilateral salpingo-oophorectomy, sacrospinous fixation, anterior and pelvic repair; posterior floor vaginal brachytherapy and 25 fractions of external beam radiotherapy | Four months after completion of radiotherapy showed that there was a tumor recurrence at the vaginal vault with bilateral hydronephrosis and died a few months later |
| 12 | Tan, 2021, (34) | 72 | Vaginal cancer | Ring pessary; NA | III | 10 years | A foul smelling friable fungating mass on the left vaginal wall measuring 5 cm × 3 cm | Six cycles of neoadjuvant chemotherapy with paclitaxel and carboplatin | Prior to the planned surgery, she had atrial fibrillation and died |
| 13 | Tan, 2021, (34) | 98 | Vaginal cancer | Ring pessary; 71 mm | IV | 7 years | A friable induration measuring 4 cm × 3 cm was seen in the posterior fornix | The patient declined further imaging investigation | Died about a year later |
POP, pelvic organ prolapse; NA, not available; AUC, area under the curve.
Conclusions
In order to avoid the occurrence of adverse events, gynecologists and caregivers should inform pessary users in detail about the standard care of the pessary and the necessity of regular follow-up. All patients need to undergo cervical cancer prevention screening and endometrial ultrasound examination prior to placement of the vaginal pessary to rule out cervical and endometrial lesions and to examine periodically so that adverse effects can be dealt with early. Local estrogen therapy can be recommended properly in conjunction with pessary use for postmenopausal women. Future studies are need to identify consensus recommendations of follow-up and complication management and the effect of local estrogen therapy on reducing pessary related complications and to develop patient-specific pessaries for different individuals to offer appropriate treatment options, thus improving patients’ satisfaction with pessary use.
Acknowledgments
The authors thank Dr. Wei Jiang for assistance with providing relevant professional images.
Funding: The Fundamental Research Funds for the Central Universities (SCU2022F4080).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-25/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-25/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-25/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of hospital Ethics Committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zeiger BB, da Silva Carramão S, Del Roy CA, et al. Vaginal pessary in advanced pelvic organ prolapse: impact on quality of life. Int Urogynecol J 2022;33:2013-20. [Crossref] [PubMed]
- Fernando RJ, Sultan AH, Thakar R, et al. Management of the neglected vaginal ring pessary. Int Urogynecol J Pelvic Floor Dysfunct 2007;18:117-9. [Crossref] [PubMed]
- Umachanger JK, Marcussen ML, Bøggild H, et al. First-line treatment of pelvic organ prolapse and discontinuation of pessary treatment. Int Urogynecol J 2020;31:1813-9. [Crossref] [PubMed]
- Bugge C, Adams EJ, Gopinath D, et al. Pessaries (mechanical devices) for managing pelvic organ prolapse in women. Cochrane Database Syst Rev 2020;11:CD004010. [PubMed]
- O'Dell K, Atnip S. Pessary care: follow up and management of complications. Urol Nurs 2012;32:126-36, 145; quiz 137. [Crossref] [PubMed]
- Harvey MA, Lemieux MC, Robert M, et al. Guideline No. 411: Vaginal Pessary Use. J Obstet Gynaecol Can 2021;43:255-266.e1. [Crossref] [PubMed]
- Brown CA, Pradhan A, Pandeva I. Current trends in pessary management of vaginal prolapse: a multidisciplinary survey of UK practice. Int Urogynecol J 2021;32:1015-22. [Crossref] [PubMed]
- Lone F, Thakar R, Sultan AH, et al. A 5-year prospective study of vaginal pessary use for pelvic organ prolapse. Int J Gynaecol Obstet 2011;114:56-9. [Crossref] [PubMed]
- Bai SW, Yoon BS, Kwon JY, et al. Survey of the characteristics and satisfaction degree of the patients using a pessary. Int Urogynecol J Pelvic Floor Dysfunct 2005;16:182-6; discussion 186.
- Hanson LA, Schulz JA, Flood CG, et al. Vaginal pessaries in managing women with pelvic organ prolapse and urinary incontinence: patient characteristics and factors contributing to success. Int Urogynecol J Pelvic Floor Dysfunct 2006;17:155-9. [Crossref] [PubMed]
- Thornton CA, Harrison RF. Unusually rapid incarceration of a polyvinyl ring pessary. Ir J Med Sci 1977;146:116. [Crossref] [PubMed]
- Poma PA. Management of incarcerated vaginal pessaries. J Am Geriatr Soc 1981;29:325-7. [Crossref] [PubMed]
- Whitworth JS, Thijs I, Bhal PS. Rapid incarceration of a ring pessary with its safe and immediate removal. J Obstet Gynaecol 2002;22:225-6. [PubMed]
- Chou YC, Yu KJ. Entrapped vaginal pessary presented with frequency and urge incontinence. J Chin Med Assoc 2003;66:181-3. [PubMed]
- Liang SJ, Chow PK, Chou SY, et al. Incarcerated vaginal pessary: A rare complication. Taiwan J Obstet Gynecol 2004;43:149-50. [Crossref]
- Ka Yu T, Ting Chung P. Cervical incarceration by ring pessaries. Acta Obstet Gynecol Scand 2004;83:313-4. [Crossref] [PubMed]
- Nallendran V, Hannah L, Watson AJ. Neglected vaginal ring pessary. J Obstet Gynaecol 2006;26:274-5. [Crossref] [PubMed]
- Govind A, Lakhi N. The enigma of early entrapment of vaginal ring pessaries. J Obstet Gynaecol 2007;27:451-2. [Crossref] [PubMed]
- Sankar A, Aziz A, Trotter P, et al. Outpatient management of incarcerated ring pessary: Use of orthopaedic bone cutters. J Obstet Gynaecol 2008;28:245-6. [Crossref] [PubMed]
- Berger J, Van den Bosch T, Deprest J. Impaction after partial expulsion of a neglected pessary. Obstet Gynecol 2009;114:468-70. [Crossref] [PubMed]
- Dasari P, Sagili H. Incarcerated foreign body in the vagina--a metal bangle used as a pessary. BMJ Case Rep 2012;2012:bcr0120125596. [Crossref] [PubMed]
- Thubert T, Deffieux X. Inside out: On rare occasions, ring pessaries can cause genital incarceration. Am J Obstet Gynecol 2014;210:278.e1. [Crossref] [PubMed]
- Manivasakan J, Arounassalame B. Encapsulated vaginal pessary. Int J Reprod Contracept Obstet Gynecol 2013;2:458-9. [Crossref]
- Jain M, Rani J, Sehgal A. Neglected vaginal pessary. Int J Reprod Contracept Obstet Gynecol 2014;3:291-2. [Crossref]
- Andrikopoulou M, Lazarou G. Rare case of neglected pessary presenting with concealed vaginal hemorrhage. Female Pelvic Med Reconstr Surg 2015;21:e1-2. [Crossref] [PubMed]
- Abdool Z. Entrapment of a vaginal ring pessary: Case report and review of the literature. S Afr J Obstet Gynaecol 2015;21:14-5. [Crossref]
- Cabral Ribeiro J, Leite C. A curious cause of pseudo-haematuria: a neglected vaginal pessary. BMJ Case Rep 2017;2017:bcr2017219690. [Crossref] [PubMed]
- Ghanbari Z, Deldar-Pesikhani M, Eftekhar T, et al. Neglected Pessary in Patient With Pelvic Organ Prolapse: A Case Report. J Family Reprod Health 2019;13:173-5. [Crossref] [PubMed]
- Pereira GMV, de Araújo CC, Juliato CRT, et al. Incarcerated Ring Pessary Repair under Local Anesthesia. J Minim Invasive Gynecol 2021;28:1121-2. [Crossref] [PubMed]
- Russell JK. The dangerous vaginal pessary. Br Med J 1961;2:1595-7. [Crossref] [PubMed]
- Martin C, Hong L, Siddighi S. What is hiding behind the pessary? Int Urogynecol J 2013;24:873-5. [Crossref] [PubMed]
- Jain A, Majoko F, Freites O. How innocent is the vaginal pessary? Two cases of vaginal cancer associated with pessary use. J Obstet Gynaecol 2006;26:829-30. [Crossref] [PubMed]
- Akino N, Wada-Hiraike O, Matsumoto Y, et al. Vaginal cancer possibly caused by pessary and immunocompromised condition: Multiple risk factors may influence vaginal cancer development. J Obstet Gynaecol Res 2016;42:748-51. [Crossref] [PubMed]
- Tan ACC, Faiz MJ. Case series: Vaginal pessary for pelvic organ prolapse and its association with vaginal cancer. Med J Malaysia 2021;76:910-3. [PubMed]
- Schraub S, Sun XS, Maingon P, et al. Cervical and vaginal cancer associated with pessary use. Cancer 1992;69:2505-9. [Crossref] [PubMed]
- Dawkins JC, Lewis GK, Toy EP. Cervical cancer complicating pelvic organ prolapse, and use of a pessary to restore anatomy for optimal radiation: A case report. Gynecol Oncol Rep 2018;26:14-6. [Crossref] [PubMed]
- Vanichtantikul A, Tharavichitkul E, Chitapanarux I, et al. Treatment of Endometrial Cancer in Association with Pelvic Organ Prolapse. Case Rep Obstet Gynecol 2017;2017:1640614. [Crossref] [PubMed]
- Bouchard ME, Rousseau E, Fortier LC, et al. Pathophysiology of Vaginal Erosions in Women Using Pessary: A Pilot Study Examining Vaginal Microbiota. J Obstet Gynaecol Can 2021;43:943-8. [Crossref] [PubMed]
- Dessie SG, Armstrong K, Modest AM, et al. Effect of vaginal estrogen on pessary use. Int Urogynecol J 2016;27:1423-9. [Crossref] [PubMed]
- Ai F, Wang Y, Wang J, et al. Effect of estrogen on vaginal complications of pessary use: a systematic review and meta-analysis. Climacteric 2022;25:533-42. [Crossref] [PubMed]
Cite this article as: Chen Q, Fang F, Lei Y, Zhang H, Zhao Z, Miao Y. Adverse events in women with neglected vaginal pessaries for pelvic organ prolapse: a case report and literature review. Gynecol Pelvic Med 2023;6:34.