Retroperitoneal sentinel lymph node biopsy by transvaginal natural orifice transluminal endoscopic surgery in early stage endometrial cancer: a video
Highlight box
Surgical highlights
• This is a new surgical method for pelvic sentinel lymph node resection without entering into the abdominal cavity.
• Transvaginal retroperitoneal sentinel lymph node resection can avoid the interference of the intestine in the surgery, as well as the damage caused by the surgery to the intestine.
What is conventional and what is novel/modified?
• The traditional sentinel lymph node resection for endometrial cancer is performed transabdominal laparoscopy. In recent years, transvaginal natural orifice transluminal endoscopic surgery (vNOTES) technology has been widely used by gynecologist surgeons in gynecological benign diseases and early malignant tumors, especially in early endometrial cancer. But these surgeries are all performed through the transperitoneal approach, and we are exploring a new surgical method, the retroperitoneal vNOTES sentinel lymph node resection, which may be a safer and more minimally invasive surgical method.
What is the implication, and what should change now?
• With the application of vNOTES in gynecological tumors, gynecological oncologists are exploring more minimally invasive methods to reduce surgical complications. The method we proposed in this study may be a good attempt to make it safer and minimally invasive for early cancer patients. Of course, this also poses new challenges for gynecologists, such as how to successfully establish a retroperitoneal space and how to successfully separate blood vessels, nerves, and lymph nodes in the retroperitoneal space.
Introduction
Endometrial cancer is the second most common cancer in developing countries. Surgical staging is often the main treatment strategy for it. When technically feasible, minimally invasive surgery (laparoscopy or robotics) is the preferred surgical method. Laparoscopic surgery has the advantages of less trauma, less bleeding during operation, and quick recovery after operation. Compared with traditional laparoscopy, staging surgery for endometrial cancer under transvaginal natural orifice transluminal endoscopic surgery (vNOTES) can effectively reduce surgical-related complications (1-4). Sentinel lymph node biopsy (SLNB) has been widely used in the surgical staging of early endometrial cancer (5-7). SLNB by vNOTES is mainly performed through the transperitoneal approach, and there have been reports of attempts to perform SLNB through the retroperitoneal approach. In 2019, Baekelandt (8) at first introduced this new retroperitoneal method by vNOTES, believing that this method was more conducive to exposing the retroperitoneal space including the iliac vessels, the tail of the obturator space, and the sacral plexus. Although the retroperitoneal approach seems to be able to better expose pelvic lymph nodes, there are few reports of this technique in the literature of endometrial cancer staging surgery except some case reports and case series reports (8-11). Retroperitoneal SLNB by vNOTES in endometrial cancer is still in the exploration stage.
In the case reported here, the patient was a 42-year-old female who was hospitalized for “irregular vaginal bleeding for 3 months”. Hysteroscopy endometrial biopsy revealed “atypical hyperplasia of the endometrium, local endometrial cancer”. This patient had no family history of tumor and Lynch syndrome, and no relevant genetic testing was performed. We performed retroperitoneal SLNB, total hysterectomy, and bilateral appendectomy by vNOTES. In this video, we introduce the operation process of retroperitoneal SLNB vNOTES in detail, and explore its feasibility and safety in early endometrial cancer. We present this article in accordance with the SUPER reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-4/rc).
Preoperative preparations and requirements
The preoperative preparation of the patient was the same as that of conventional vaginal endoscopic surgery. The day before the operation, the patient had a light diet, used sodium phosphate to clean the intestinal tract, and used antibiotic cefazolin sodium 1 g intravenously half an hour before the operation to prevent infection. Surgical instruments: special internal diameter 5 cm vNOTES port (HangT Port; Beijing HangTian KaDi Technology R&D Institute, Beijing, China), laparoscopic near infrared (NIR) fluorescent optic device (TC 300, Karl Storz®, Germany), and other conventional laparoscopic instruments.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
The patient was placed in dorsal lithotomy position, and a urinary catheter was placed after general anesthesia with tracheal intubation.
Step-by-step description
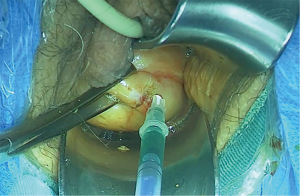
Step 1: a total of 2 mL of indocyanine green (ICG) solution at a 1.25 mg/mL concentration was injected into the cervix at the 3 and 9 o’clock positions 15 min before surgery (Figure 1).
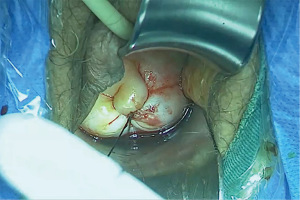
Step 2: No. 4 silk suture was used to suture the exocervix to prevent tumor spreading (Figure 2).
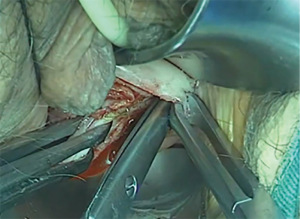
Step 3: establishment of retroperitoneal space.
- Circumferentially cut the vaginal wall 0.5 cm below the cervical vaginal junction, passively separate the retroperitoneal space along the left fornix incision towards the pelvic side wall, and enter the obturator fossa (Figure 3).
- Insert a 24-F catheter into the obturator fossa, and inject 60 mL physiological saline into the balloon to expand the potential space.
- Insert the vNOTES port with a diameter of 5 cm inner ring into the retroperitoneal cavity, place a support device in the vagina to avoid the prolapse of the vNOTES port inner ring, connect the sealing cover, and maintain the CO2 pressure in the retroperitoneal space to 8–10 mmHg.
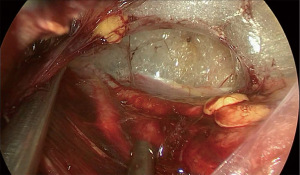
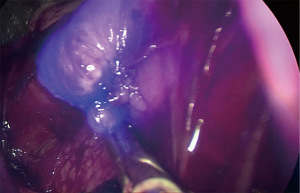
Step 4: resection of pelvic sentinel lymph nodes.
- We use conventional laparoscopic instruments for operation. The obturator nerve, ureter, external iliac vessels, and internal iliac vessels were identified by careful dissection from the tail of the obturator fossa (Figure 4).
- Sentinel lymph node (SLN) were identified and removed by careful dissection (Figure 5).
- Then the same operation was performed on the opposite side.
The surgical process was displayed in the video (Video 1).
Subsequently, the operation was completed through vagina-assisted vNOTES hysterectomy and bilateral salpingo-oophorectomy. Absorbable sutures were used to close the vaginal vault from the anterior to the posterior vaginal wall.
Postoperative considerations and tasks
The operation lasted 116 minutes and the patient lost 90 mL of blood. The patient was discharged and started with a liquid diet 6 hours after surgery. The urinary catheter was removed on the first postoperative day and the patient was discharged 2 days after surgery. The final pathological report showed that differentiated endometrial carcinoma in the uterus, infiltrating the superficial layer of the muscle wall (<1/2 layer of the muscle wall), without definite vascular cancer thrombi or nerve invasion. There were four left pelvic lymph nodes and four right pelvic lymph nodes were resected, all of which were negative. The patient was followed up for 12 months without complications.
Tips and pearls
- The establishment of retroperitoneal space is the key to successful surgery.
- If the establishment of retroperitoneal space fails, intraperitoneal surgery through vNOTES or abdominal wall is still a reliable remedial measure.
Discussion
The traditional surgical methods for endometrial cancer are transabdominal laparoscopic pelvic lymphadenectomy, hysterectomy, and bilateral ovariosalpingectomy. In recent years, with the exploration of more noninvasive surgical methods, vNOTES technology has been widely used by gynecologist surgeons in gynecological benign diseases and early malignant tumors, especially in early endometrial cancer, and proved its reliabilities. SLNB can not only improve surgical outcomes, but also retain reliable surgical staging results. However, these lymph node resection methods all enter the abdominal cavity for lymph node resection or sampling. Since Baekelandt (8) at first tried transvaginal retroperitoneal sentinel lymph node resection, gynecologists have seen another potentially more advantageous surgical approach.
The retroperitoneal SLNB by vNOTES may be feasible for early endometrial cancer. Since retroperitoneal SLNB does not need to enter the abdominal cavity, compared with transperitoneal vNOTES, it may have the following advantages: first, for the patient, the obturator fossa can be easily accessed through the retroperitoneal vNOTES approach, where the blood vessels and nerves can be well exposed. For the access is next to the cervix, the afferent lymph vessels and the true sentinel lymph nodes, which are the stained lymph nodes closest to the tumor can be directly identified. Since SLN is most common in the external iliac or obturator region of patients with endometrial cancer, SLNB is more likely to be performed via a retroperitoneal approach. When identifying internal iliac blood vessels, uterine arteries can also be coagulated, which can reduce bleeding during hysterectomy. Second, retroperitoneal SLNB can be achieved through lower CO2 pressure and no Trendelenburg tilt, which reduces the impact on patients’ cardiopulmonary function, even for the elderly and obese patients, this seems to be feasible. What’s more, the retroperitoneal SLNB is not distracted by the intestinal tract and the pelvic adhesion patients with previous abdominopelvic surgeries. At the same time, it can also avoid bowel injury, has little interference with the intestinal tract, and will not leave scars leading to pelvic adhesion, which offers greater benefits to obese patients, advanced age, and previous abdominopelvic surgeries patients.
Although this approach has many advantages, we acknowledge that it also has some key limitations. Failure to establish a retroperitoneal space, peritoneal rupture, and vascular injury are still the main reasons for conversion to transperitoneal surgery. During the establishment of retroperitoneal space, peritoneal rupture should be avoided as much as possible. The establishment of retroperitoneal space is the key to the success of the operation. In addition, the chopstick effect of the instrument and the limited operating space are still the main difficulties in the retroperitoneal approach by vNOTES, but these difficulties can be overcomed by adequate training of surgeons and the use of articulating instruments.
Conclusions
The retroperitoneal SLNB by vNOTES is an innovative attempt in patients with early endometrial cancer. This method has many advantages, but there are also some limitations, and the feasibility and safety of this method need more research to prove.
Acknowledgments
The video was awarded the second prize in the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery).
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-4/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-4/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-4/coif). The series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this manuscript and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang Y, Deng L, Tang S, et al. vNOTES Hysterectomy with Sentinel Lymph Node Mapping for Endometrial Cancer: Description of Technique and Perioperative Outcomes. J Minim Invasive Gynecol 2021;28:1254-61. [Crossref] [PubMed]
- Tantitamit T, Lee CL. Application of Sentinel Lymph Node Technique to Transvaginal Natural Orifices Transluminal Endoscopic Surgery in Endometrial Cancer. J Minim Invasive Gynecol 2019;26:949-53. [Crossref] [PubMed]
- Lee CL, Liu HM, Khan S, et al. Vaginal natural orifice transvaginal endoscopic surgery (vNOTES) surgical staging for endometrial carcinoma: The feasibility of an innovative approach. Taiwan J Obstet Gynecol 2022;61:345-52. [Crossref] [PubMed]
- Li Y, Hou Q, Gong Z, et al. Sentinel Lymph Node Mapping and Staging Surgery Via Gasless Transvaginal Natural Orifice Transluminal Endoscopic Surgery: A Case Report of an Endometrial Cancer Patient and Comorbid Rheumatic Heart Disease. Am J Case Rep 2022;23:e936694. [Crossref] [PubMed]
- Persson J, Salehi S, Bollino M, et al. Pelvic Sentinel lymph node detection in High-Risk Endometrial Cancer (SHREC-trial)-the final step towards a paradigm shift in surgical staging. Eur J Cancer 2019;116:77-85. [Crossref] [PubMed]
- Hagen B, Valla M, Aune G, et al. Indocyanine green fluorescence imaging of lymph nodes during robotic-assisted laparoscopic operation for endometrial cancer. A prospective validation study using a sentinel lymph node surgical algorithm. Gynecol Oncol 2016;143:479-83. [Crossref] [PubMed]
- Zuo J, Wu LY, Cheng M, et al. Comparison Study of Laparoscopic Sentinel Lymph Node Mapping in Endometrial Carcinoma Using Carbon Nanoparticles and Lymphatic Pathway Verification. J Minim Invasive Gynecol 2019;26:1125-32. [Crossref] [PubMed]
- Baekelandt JF. New Retroperitoneal Transvaginal Natural Orifice Transluminal Endoscopic Surgery Approach to Sentinel Node for Endometrial Cancer: A Demonstration Video. J Minim Invasive Gynecol 2019;26:1231-2. [Crossref] [PubMed]
- Huber D, Hurni Y. Sentinel Node Biopsy for Endometrial Cancer by Retroperitoneal Transvaginal Natural Orifice Transluminal Endoscopic Surgery: A Preliminary Study. Front Surg 2022;9:907548. [Crossref] [PubMed]
- Mathey MP, Romito F, Huber DE. Retroperitoneal Sentinel Lymph Node Biopsy by Vaginally Assisted Natural Orifices Endoscopic Transluminal Endoscopic Surgery in Early Stage Endometrial Cancer: Description of Technique and Surgeon's Perspectives after the First Experience. Case Rep Oncol 2022;15:291-9. [Crossref] [PubMed]
- Comba C, Demirayak G, Simsek C, et al. Transvaginal natural orifice transluminal endoscopic surgery (VNOTES) total retroperitoneal sentinel lymph node biopsy for an endometrial cancer patient with prior colon cancer surgery. Int J Gynecol Cancer 2021;31:1386-7. [Crossref] [PubMed]
Cite this article as: Li Y, He L, Hou Q, Zhang Q, Gu D, Lin Y. Retroperitoneal sentinel lymph node biopsy by transvaginal natural orifice transluminal endoscopic surgery in early stage endometrial cancer: a video. Gynecol Pelvic Med 2023;6:25.