Whole extraperitoneal sacral hysteropexy by transvaginal natural orifice transluminal endoscopic surgery
Highlight box
Surgical highlights
• While traditional surgery is done in the abdominal cavity, the new surgery is done in the extraperitoneal, without interference from the abdominal cavity.
What is conventional and what is novel/modified?
• The traditional surgery is to open the peritonaeum in front of the sacral promontory and the right pelvic peritoneum. The long arm of the mesh is sutured to the anterior longitudinal ligament of S1, then the short arm of the mesh is sutured to the cervix.
What is the implication, and what should be change now?
• The new procedure can be performed completely extraperitoneally with transvaginal natural orifice transluminal endoscopic surgery, and is free of intestinal influence during and after surgery, resulting in faster postoperative recovery and less pain without abdominal wall incisions.
Introduction
Pelvic organ prolapse is one of the common diseases in women, surgery is the main treatment for patients with severe symptoms. Sacrocolpopexy remains the gold standard among the surgical modalities for apical prolapse. Sacral hysteropexy is most commonly used for young patients who do not wish to undergo hysterectomy (1,2). This procedure, in which the cervix is attached to the anterior longitudinal ligament of the first sacrum via Y-shaped mesh, has a low recurrence rate.
At present, there are many reports on laparoscopic and vaginal surgical approach. Traditional sacral hysteropexy is mostly performed under laparoscope, and there are many reports on laparoscopic and vaginal surgical approach (3). We reported a new surgical approach—whole extraperitoneal approach by transvaginal natural orifice transluminal endoscopic surgery (v-NOTES), the surgery was completed completely in the extraperitoneal space. This is a 38-year-old young woman, was admitted to the hospital after 2 years of uterine prolapse. The operation lasted 156 minutes, no massive bleeding occurred during the operation. Point C was −5, and no infection, mesh exposure, erosion and other complication occurred at 6 months follow-up. We present this article in accordance with the SUPER reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-11/rc).
Preoperative preparations and requirements
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this manuscript and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Vaginal irrigation 2 days before operation. We gave the patient a prophylactic antibiotic 30 minutes before surgery. The mesh was copiously irrigated intraoperative.
Step-by-step description
- The patients were placed at lithotomy position of bladder with urethral catheter indwelled after general anesthesia.
- Transversely incise the posterior fornix of vagina without opening the peritoneum, perform a blunt dissection for separation in the right pararectal space, the finger is palpable on the right ischiatic spine as a sign. Place a 24 Fr double-lumen balloon urinary catheter in the space after blunt separation, inject the water, sufficient expansion of the balloon can establish the initial shape of the extraperitoneal space. Place a laparoscopic instrument for v-NOTES in the extraperitoneal space. Considering the difficulty of fixing the conventional incision retractor (inner ring diameter 8 cm), a small inner ring (diameter about 4.5 cm) was placed in the outer peritoneum as the base of the incision retractor, with a patented vaginal sleeve fixing the incision retractor additionally, and the pneumoperitoneum space is established extraperitoneal.
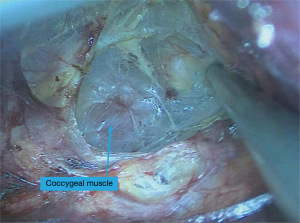
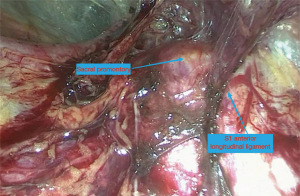
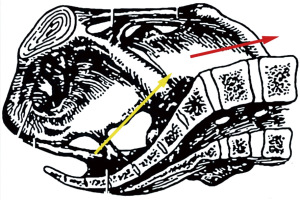
- The extraperitoneal space was separated under the pneumoperitoneum to the sacral promontory. The separation is performed in a loose interstitial space cephalad from the right side of the rectum along the lateral wall of the pelvis. It is easy to get lost in the extraperitoneal space, the coccygeus can be seen on the medial side of the ischial spine (Figure 1), and the medial side of the coccygeus is the sacrum, which separates to the sacral promontory cephalically along the sacral curve. Changes in the direction of the bony structure can help us to determine whether the promontory area has been reached (the separation direction initially inclines to the ventral side along the sacral arc, and when the separation direction turns to the side of the head along the bony structure, the sacral promontory is reached) (Figures 2,3
). - After the mesh access was established, anatomical markers for sacral promontory, anterior longitudinal ligament, median sacral vessel may be fully exposed.
- Then suture the long arm of the Y-shaped mesh on the anterior longitudinal ligament of the first sacra. Suture in narrow extraperitoneal space is difficult, usually 2 to 3 stitches, and the mesh is fully flattenned.
- The vaginorectal space and vaginovesical space were separated, pull out the mesh, suturing and fixating the short arm of the mesh around the cervix, the mesh should be tension-free.
- Sutures the vaginal incision, the whole mesh was located extraperitoneally. Gauze was inserted into the vagina, which may help the stick between vaginal wall and the mesh.
The whole procedure is shown in Video 1.
Postoperative considerations and tasks
After the patient recovered from anesthesia, normal diet is started. The urinary catheter is removed 24 hours later and the vaginal gauze is removed 24 hours later. Prophylactic antibiotics were given for 48 hours after surgery. Discharge 72 hours after surgery.
Tips and pearls
During the separation of the extraperitoneal space, be careful not to rupture the peritoneum, after peritoneum rupture, transabdominal laparoscopic surgery is required.
Suture at the anterior longitudinal ligament of S1 has a risk of vascular injury, and hemostatic instruments should be prepared to prevent bleeding.
Discussion
The surgical approach under v-NOTES has been widely used in Gynecological surgery. It has also been reported frequently in pelvic floor dysfunction diseases. In 2022, Lu et al. (4) reported standard practice of presacral exposure during v-NOTES for sacrocolpopexy. In this surgery, peritoneum needs to be opened before a mesh pathway is established. An important step in the procedure is to ensure that the mesh is completely extraperitoneal. In that case, why not perform this procedure outside the peritoneum?
The novel feature of our surgical video was the extraperitoneal approach. This method is performed in the extraperitoneal space without restriction of obesity, abdominal adhesion, and occlusion of bowel position, etc. The local establishment of pneumoperitoneum is also a new option for patients with cardiopulmonary diseases who cannot tolerate pneumoperitoneum pressure.
The extraperitoneal approach could clearly dissect the important tissues of the anterior sacral region, such as the sacral promontory and the presacral vessels, so as to avoid injury in the subsequent operation. Compared with traditional laparoscopy through umbilical cord, transvaginal surgery can more accurately reach the first sacral vertebra and even the second sacral vertebra. Avoid difficulty exposing the anterior longitudinal ligament of S1 due to the large angle drop of L5–S1 (mean 65 degrees). Avoid suturing to the promontory of the sacrum, especially to the L5 intervertebral disc. We have successfully tried extraperitoneal approach for sacrocolpopexy in v-NOTES with good results in a small number of patients. The extraperitoneal approach will allow more patients to be treated with less invasive surgery (5).
Although the v-NOTES approach involves a class II incision, but there is no evidence that transvaginal surgery increases postoperative infection rates. So preoperative vaginal irrigation, intraoperative aseptic operation, iodophor irrigation mesh, and rational use of antibiotics are also important (6). As the largest women’s health medical institution in the region, the surgeon hospital retrospectively analyzed nearly 2,000 cases of v-NOTES surgery, and the overall infection rate was 1.3%, and the complications of surgery-related infections did not increase (7).
At last, there are certain requirements for surgical techniques in the extraperitoneal reverse dissection. The surgeons were familiar with pelvic floor anatomy and skillful in laparoscopic single-port suture technique, which also contributed to the successful operation.
Conclusions
In conclusion, the extraperitoneal approach is a true whole-process extraperitoneal procedure under v-NOTES surgery, as a new approach for sacral hysteropexy is a feasible and safe approach.
Acknowledgments
The video was awarded the first prize in the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery).
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-11/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-11/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-11/coif). The series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)” was commissioned by the editorial office without any funding or sponsorship. Y.L. reports that the vaginal sleeve used to secure a vaginal incision retractor is patented, of which the inventor is Y.L. and the patentee is Chengdu Women and Children’s Central Hospital. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this manuscript and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Campagna G, Vacca L, Panico G, et al. Laparoscopic sacral hysteropexy versus laparoscopic sacral colpopexy plus supracervical hysterectomy in patients with pelvic organ prolapse. Int Urogynecol J 2022;33:359-68. [Crossref] [PubMed]
- Maldonado PA, Jackson LA, Florian-Rodriguez ME, et al. Comparisons of Functional Apical Support After Sacral Hysteropexy Versus Sacral Colpopexy: A Cadaveric Study. Female Pelvic Med Reconstr Surg 2020;26:664-7. [Crossref] [PubMed]
- Liu J, Kohn J, Sun B, et al. Transvaginal Natural Orifice Transluminal Endoscopic Surgery Sacrocolpopexy: Tips and Tricks. J Minim Invasive Gynecol 2019;26:38-9. [Crossref] [PubMed]
- Lu Z, Hua K, Chen Y, et al. Standard practice of presacral exposure during transvaginal natural orifice transluminal endoscopic surgery for sacrocolpopexy. BJOG 2022;129:1004-7. [Crossref] [PubMed]
- Gu D, Huang L, Feng D, et al. The Pure Extraperitoneal Approach for Sacrocolpopexy in Transvaginal Natural-Orifice Transluminal Endoscopic Surgery. J Gynecol Surg 2023;39:108-13. [Crossref] [PubMed]
- Illiano E, Trama F, Crocetto F, et al. Prolapse Surgery: What Kind of Antibiotic Prophylaxis Is Necessary? Urol Int 2021;105:771-6. [Crossref] [PubMed]
- Hou Q, Li X, Li Y, et al. Analysis and suggestions on the complications in 2000 cases of transvaginal natural orifice transluminal endoscopic surgery: Can it be a conventional surgery? Int J Gynaecol Obstet 2023; Epub ahead of print. [Crossref] [PubMed]
Cite this article as: Gu D, He L, Lin Y. Whole extraperitoneal sacral hysteropexy by transvaginal natural orifice transluminal endoscopic surgery. Gynecol Pelvic Med 2023;6:24.