
Surgical technique of robotic Piver class III hysterectomy with preserving ureteral branch of uterine artery on early-stage invasive cervical cancer
Highlight box
Surgical highlights
• It’s a new method of radical hysterectomy for cervical cancer by preserving the ureteral branch of the uterine artery.
• This is a robot-assisted laparoscopic surgery.
What is conventional and what is novel/modified?
• Separation of the uterine artery and the ureteral branch of the uterine artery are important components of dividing the vesicouterine ligament. Precise identification of anatomy of the vesicouterine ligament and dividing of it has been difficult to obtain.
• We provide a method of dissection of the ureteral branch of the uterine artery and a new method of cutting off the uterine artery via robot-assisted minimally invasive surgery (MIS) quickly and safely.
What is the implication, and what should change now?
• Preserving the ureteral branch of the uterine artery helps preserve the blood supply of the ureter.
• Due to the advantages of three-dimensional vision, high definition, greater precision, and greater ergonomic potential, robotic-assisted MIS makes this procedure safer and more feasible.
Introduction
Cervical cancer is the most frequently occurring cancer of gynecological malignancies in women around the world, and also a serious threat to women’s reproductive health (1). Radical hysterectomy and plus pelvic lymph node dissection are the primary methods of treatment for patients suffered from early-stage cervical cancer (2). Conventional radical hysterectomy is a most important part of the surgical procedure. Due to complications leading to morbidity and mortality increasing with radicality, it is recommended that the dimensions of the removed parametrium adapted according to the factors affecting recurrence in cervical cancer to obtain more appropriate surgical margins (3). Owing to the regularity of pelvic lymph node metastasis of cervical cancer, pelvic sentinel lymphadenectomy is an alternative to pelvic lymphadenectomy. The published data has shown that both 5-year disease-free survival and overall survival rate after sentinel lymph node biopsy alone are higher than 90% and do not differ from pelvic lymphadenectomy survival data (4).
The surgical approach depends on the operation indication and condition of the patient, the surgeon’s operative style and skills, and patient’s willingness. Over the past decade, there has been increasing evidence supporting the adoption of minimally invasive surgery (MIS) and it was widely used by gynecological oncologists for cervical cancer surgery. Compared with the abdominal radical hysterectomy, MIS is associated with less blood loss, shorter hospital stay, better cosmesis, faster recovery, and comparative effectiveness with respect to oncological outcomes, making hysterectomy an intervention with less emotional impact (5-7). However, in 2018, the publication of the results of the phase III, randomized Laparoscopic Approach to Cervical Cancer (LACC) trial highlighted that the execution of minimally invasive radical hysterectomy correlates with an increased risk of recurrence and death compared to laparotomy (8). In recent years, the application of robotic approach has gradually increased and received more and more attention and has demonstrated its unique advantages including three-dimensional vision, high definition, greater precision in the fields of cervical cancer surgery without an increased risk of worse oncologic outcomes (9). The clinical outcomes following robotic radical hysterectomy have been well documented in some studies (10,11).
The procedure of parametrium tissue excision, is associated with intraoperative complications such as massive bleeding and ureteral injury, and postoperative bladder dysfunction because of damage to the pelvic autonomic innervation. Separation of the anterior leaf of the vesicouterine ligament, which is so-called opening of ureteral tunnel, is the core cause of surgical difficulties and complications and blinded performed in traditional surgery. It is necessary to carefully separate the connective tissue complex, including the uterine artery, and the ureteral branch of the uterine artery to separate the anterior leaf of the vesico-uterine ligament. Studies have shown that the incidence of these complications can be reduced by preserving the ureteral branch of the uterine artery during undergoing radical hysterectomy (12). Therefore, clear exposure, precise operation, and efficient hemostasis are crucial for this surgery.
In light of the above issues, we decided to apply the technique of preserving ureteral branch of the uterine-artery radical hysterectomy via robot-assisted minimally surgery for a patient with early-stage cervical cancer. This method makes parametrium tissue excision more accurate and easier, and facilitating rapid postoperative recovery. In this case, the whole operation took 220 minutes and estimated blood loss was 50 mL. Two weeks later, the ureter was successfully removed. We present this article in accordance with the SUPER reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-5/rc).
Preoperative preparations and requirements
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Patient preparation
A 40-year-old woman was admitted to our hospital due to vaginal bleeding after sexual intercourse for 2 months. The screening test for cervical cancer before admission showed that the high-risk human papilloma virus (HR-HPV) testing was negative, and the atypical glandular epithelial cells were found in the cervical thinprep cytology test (TCT). Further colposcopy with targeted biopsy revealed cervical adenocarcinoma. The pelvic magnetic resonance imaging (MRI) results showed a mass of approximately 26 mm × 27 mm × 20 mm in size on the posterior wall of the cervix, and no abnormalities were found in the rest. Combined with physical examination results, the clinical stage IB cervical adenocarcinoma was diagnosed after admission. We performed thoroughly preoperational communication with the patient and her relevants, eventually robot-assisted laparoscopic radical surgery for cervical cancer was chosen for the treatment.
Vaginal scrubbing (1% povidone-iodine) was performed two days before surgery. Cleaning and disinfection of navel skin and preoperative bowel through oral sodium phosphate solution was performed 1 day before surgery.
Instrumental requirements
Da Vinci Xi Surgical Robot, monopolar electrode scissors and bipolar coagulation (Xi, Intuitive Surgical, Sunnyvale, CA, USA), and 24-F foley catheter are required.
Surgical team
Two gynecologic oncologists, two experienced gynecologic surgical nurses and an anesthesiologist proficient in general anesthesia. The operator is a surgeon with 30 years of experience in gynecological malignancy surgery and has experience in over 100 robotic surgeries for gynecological diseases. The assistant is a surgeon with 17 years of experience gynecological malignancy surgery and has experience in over 20 robotic surgeries for gynecological diseases.
Instrumental requirements
Da Vinci Xi Surgical Robot, monopolar electrode scissors and bipolar coagulation, and 24-F foley.
Patient position
The patient was placed in the bladder lithotomy position. All procedures were performed under general anesthesia.
Step-by-step description
This surgery was completed on November 3, 2022. The detailed surgical procedures of Piver class III hysterectomy with ureteral branch of uterine artery preservation included the following 10 steps.
Step 1
Paraaortic lymphadenectomy, bilateral pelvic lymphadenectomy following routine procedures. After pelvic lymphadenectomy, the ureter was dissected inferiorly.
Step 2
Uncovering of the paravesico fossa and the pararectal fossa in between the ureter and the internal iliac artery. The uterine artery was identified and located by pulling the atresia side of the umbilical artery. While exposing by using robot bipolar forceps to pull the internal iliac artery or uterine artery, or the fascia on the surface of the ureter or using bipolar forceps or unipolar scissors to parry important organs, the surgeon separated fascia tissue to uncover the paravesico fossa and the pararectal fossa in between the ureter and the internal iliac artery to complete ureteric dissection up to the so-called ureteral tunnel by using either electrosurgical separation or non-charged blunt separation methods of unipolar scissors. At the same time, the assistant used traditional laparoscopic tissue forceps to clamp and pull the uterus to assist in exposure.
Step 3
Posterior dissection with division of the uterosacral ligament approximately 2 cm from the uterine insertion. We utilised similar methods of exposure and separation as described in the above step in this process. The methods for exposing and separating in the following steps also complied with this approach. Besides, larger blood vessels were first electrocoagulated with bipolar forceps and then electrically cut off with unipolar scissors.
Step 4
Skeletonization of the uterine artery and its urethral branch. After further dissociating the ureter from the posterior lobe of the broad ligament, the surgeon continued to separate the fascia around the uterine artery and some of the fascia on the surface of the ureter until the ureteral branch of the uterine artery between them was clearly exposed (Figure 1).
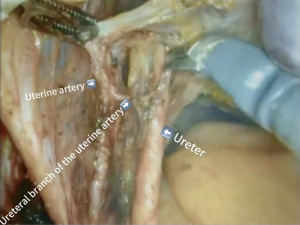
Step 5
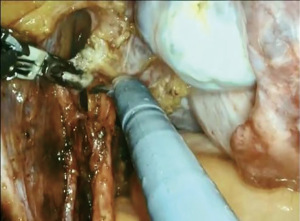
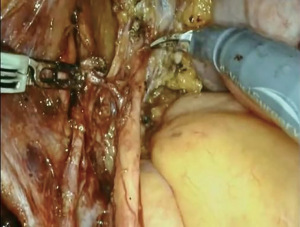
Coagulation and section of the uterine artery below the ureteral branch. After excising connective and adipose tissue around, we isolated the ureteral branch of the uterine artery running cranially from the uterine artery to the ureter and utilised bipolar clamp to electrocoagulate of the uterine artery below the ureteral branch, while using scissors to ward off the ureter. Upon confirming that it has been completely coagulated, the condensed area of uterine artery was electrically cut off by unipolar scissors (Figures 2,3). When sectioning the uterine artery, assurance of thorough coagulation is crucial to prevent intraoperative and postoperative bleeding. Bleeding at this site can be challenging to manage due to limited access.
Step 6
Opening of vesico peritoneal fold and detaching bladder downward. When the assistant pulled the uterus towards the cephalad of the patient, the surgeon used unipolar scissors to electrically cut off the vesico peritoneal fold and then continued to cut the fascia between the bladder and cervix and push the bladder downwards.
Step 7
Exposure of the vesicouterine space and section of the vesicouterine ligament. When the vesico was hold by the surgeon through the bipolar clamp and the cut down proximal end of uterine artery at the uterus pulled by the assistant, the anterior leaf of the vesicouterine ligament was directly recognized and easily and safely divided by the unipolar scissors far from the ureter. Then, the surgeon gently picked up the connective tissue on the surface of the ureter, and after that, the posterior leaf of the vesicouterine ligament was clearly displayed due to the action of tension. There is an avascular area between the posterior leaf of the vesicouterine ligament and the cervix. By using the precise and efficient cutting of unipolar scissors, the posterior leaf of the vesicouterine ligament was cut along this avascular area, and the ureteral tunnel was fully detached.
Step 8
Segregation of paravaginal tissue and further dissociation of bladder. The surgeon continued to cut the connective tissue between the vagina and bladder by unipolar scissors, causing the bladder to further detached from vagina.
Step 9
Resection of 3/4 cardinal ligament and about 2 cm paracolpium and excision of approximate 3 cm vaginal tissue. Most parts of these surgical steps were those commonly practiced in conventional radical hysterectomy. The difference is that, after same procedure performed on the opposite side, the surgeon used sutures to close the vagina at the level below the upper third of the vagina before excision of vagina to avoid exposing cervical cancer tissue to the abdominal cavity, beware of no penetration into the vaginal mucosa.
Step 10
Transvaginal suture of vaginal stump. The surgeon and the assistant transferred to the patient’s caudal side to suture the stump transvaginally.
In Video 1, we presented the surgical procedures from step 3 to step 8 in detail to show how to perform robotic Piver class III hysterectomy with ureteral branch of uterine artery preservation.
Postoperative considerations and tasks
Postoperative prophylactic antibiotics were applied and pelvic drainage tubes were retained for 48 hours and removed when the drainage fluid was non bloody and less than 100 mL, and the patient had no fever or obvious abdominal pain. Due to the fact that the optimal timing for removal of transurethral catheters remains unclear and often depends on surgeon preferences (13), indwelling catheterization lasted for 14 days after radical hysterectomy by convention in our hospital. Attention should be paid to the occurrence of postoperative complications such as bleeding, infection, thrombosis, and damage to surrounding organs such as the bladder, ureter, intestines, etc. Due to the high risk of thrombosis for patients with malignancy, routine prophylactic use of enoxaparin was administered from the first day after surgery, total for one week (Daily subcutaneous injection of 4000AxaIU). The patient regained exhaust on the second day after surgery. The routine blood test showed no abnormalities on the third day after surgery. The patient showed no symptoms of fever, chest pain, lower limb pain, or vaginal discharge postoperatively. After removing the catheter, the patient successfully urinated. The patient was discharged successfully 14 days after the operation without complications. Before discharge, the patient underwent a re-examination of urinary system ultrasound, lower limb vascular ultrasound, and urine residue in bladder without any abnormalities.
According to the postoperatively pathological examination, the patient was eventually diagnosed with pathological stage IB3 cervical adenocarcinoma. She was told to go to an institution with radiation therapy equipment as soon as possible to receive adjuvant radiotherapy and chemotherapy.
The patient was informed to undergo a follow-up every 3 months for the first 2 years after treatment, every 6 months for the 3–5 years, and annually thereafter. The examination items include symptom inquiry, physical examination, gynecological ultrasound examination, vaginal cytology examination, and necessary laboratory tests. If any specific situation happened, such as vaginal bleeding, MRI or computed tomography (CT) scan should be scheduled in time.
Tips and pearls
- The intraoperative bleeding in this surgery was only 50 mL. The use of robot unipolar scissors for gentle and precise separation with electricity, the assistance of robot bipolar forceps for traction and reliable electrocoagulation, and the separation of ureteral tunnels in the avascular area are all key factors contributed to less bleeding.
- We used bipolar electrocautery to electrocoagulation the uterine artery below the ureteral branch of the uterine artery and cut it off with unipolar scissors. This protects blood perfusion of the ureter from the ureteral branch of the uterine artery. Benefits of robotic approach: three-dimensional vision, amplification effect, high definition, greater precision help to recognize the ureteral branch, which can be quite thin and easily damaged, and avoid injuries to the serous layer of the distal ureter and protect sufficient ureteral blood supply postoperatively.
Discussion
Cervical cancer is the most common gynecological malignant tumor in women worldwide. Its principal treatment methods include surgery, radiotherapy and chemotherapy. MIS has been used as the main means of surgical treatment of cervical cancer until the introduction of the significant prospective randomized phase III trial revealing superior status of open surgery to laparoscopic surgery in terms of survival benefits for cervical cancer patients in 2018 (8). However, the causes and mechanisms of possible harmful effects of MIS are still unclear and controversial. A propensity-score based analysis reported that short-term perioperative outcomes were similar after laparoscopic and open abdominal radical hysterectomy in patients with tumor <2 cm, and the adoption of MIS did not impact survival outcomes in this low-risk group (14). Similar results have also been reported in other studies (15). Compared with open surgery, MIS has the equivalent or lower operative morbidity, and has shorter hospital stay and aesthetic appearance (16,17). Therefore, MIS is still applied to surgical treatment of cervical cancer in selected patients through some improvement of non-tumor technique to reduce spillage of tumor cells without compromising surgical safety and prognosis although there was a decrease in the adoption of minimally invasive radical hysterectomy (from 58% to 42.9%) (18). The advantages of three-dimensional vision, high definition, greater precision of robotic technology (5-7), and the use of the dexterous robotic monopolar scissor for separation are in aid of better exposing the avascular space and resulted in reducing surgical bleeding and shortening the operation time, and greater ergonomic potential might allow the surgeon to function better during the operation. The MEMORY study has already demonstrated that patients with IA1 (LVSI+)-IB1 cervical cancer receiving robotic-assisted approach experienced similar oncologic outcomes than patients receiving open surgery (15). The phase III prospective Robotic-assisted Approach to Cervical Cancer (RACC) trial and the trial of Robotic Versus Open Hysterectomy Surgery in Cervix Cancer (ROCC) will further clarify the impact of robotic-assisted MIS in patients undergoing a radical hysterectomy (19).
Radical hysterectomy is one of independent factors associated with urinary complications (20). It was reported that during the surgery the ureter was injured in 1.32% of cases, whereas the percentage of bladder injuries was 1.49%. In the early postoperative period vesicovaginal or ureterovaginal fistulas appeared in 2.61% and 2.43% of cases, respectively (20). In radical hysterectomy, it is necessary to open the ureteral tunnel which is the most difficult part of the whole procedure and may lead to complications such as bleeding or ureteral injury. The procedure involves ligating the uterine artery and veins and cutting them at their origin from the internal iliac artery. This stops blood perfusion from the ureteral branch of the uterine artery and might result in insufficient ureteral blood supply and hydronephrosis postoperatively, which may result in postoperative complications, such as urinary fistula and postoperative urinary dysfunction (21). It was reported that the ureteral space was actually a potential avascular space locating medial to the ureter between the anterior leaf and posterior leaf of the vesicouterine ligament (22). Previous studies reported that the blood loss during this operation was 300–1,800 mL in traditional abdominal surgery (23). Surgically separation of the vesicouterine ligament along the avascular zone and preservation of the ureter branch from the uterine artery might help reduce the blood loss and avoid ureteral injury (24). To avoid such problems, the procedure of sparing the ureteral branch of the uterine artery in radical hysterectomy was developed (12,25). In addition, considering the rarity of parametrial involvement in low-risk cervical cancer, some researchers have questioned the necessity for extensive removal of parametrial tissue and dissection of adjacent vital structures. Tailored removal of parametrium adapted according to the factors affecting recurrence in cervical cancer might help to reduce risk of complications (3).
In our study, we successfully separated the ureteral branch of the uterine artery by means of the three-dimensional imaging and amplification effects of surgical robots and clearly exposed the avascular zone of the ureteral tunnel. This is quite different from the indocyanine green (ICG) angiography method used in another study, which demonstrated that ICG angiography could provide real-time images of the uterine artery, its ureteral branch, the ureter distal serous layer and tissue supplied by the ureteral branch (12). This technology overcome the issue of traditional surgery’s difficulty in accurately displaying this artery. However, dependency on specialized imaging equipment and allergic reaction are the limitations of this technology. Although robotic surgery also relies on equipment, it overcomes the problem of allergic reactions. The three-dimensional imaging and amplification effect of robotic surgery also makes the avascular space of the vesicouterine ligament more visible. Besides, we made the cutting of the ureteral branch of the uterine artery precisely and safely with the help of flexible rotation of the robotic arm and the precise cutting of unipolar scissors. These are the unique advantages of robotic surgery in radical hysterectomy. The intraoperative blood loss was only 50 mL, and subsequent short-term follow-up results: there was no postoperative bleeding or urinary system damage, and the bladder function recovered well in this case, confirmed that this procedure is safe and effective in reducing complications.
However, the mastery of robotic surgery also requires getting beyond the initial learning curve. In addition, application of robot would also increase the cost of surgery. There are few reports on the radical hysterectomy of cervical cancer with preserving ureteral branch of uterine artery up to now. Its impact on long-term prognosis and survival of patients needs further study.
Conclusions
With the help of three-dimensional imaging, amplification effect, flexible operation and reliable handling of blood vessels of monopolar scissors and bipolar clamps, flexible rotation of the robotic arm in robotic surgery, this new surgical procedure of robotic Piver class III hysterectomy with preserving ureteral branch of uterine artery can be done along the avascular zone in the vesicouterine ligament with less bleeding. It is safe and efficient for early-stage invasive cervical cancer.
Acknowledgments
The video was awarded the third prize in the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery).
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-5/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-5/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-5/coif). The series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [Crossref] [PubMed]
- Cohen PA, Jhingran A, Oaknin A, et al. Cervical cancer. Lancet 2019;393:169-82. [Crossref] [PubMed]
- Birge O, Bakir MS, Dogan S, et al. The Relationship Between Parametrial Involvement and Parametrial Tissue Removed in Radical Surgery in Early-Stage Cervical Cancer. World J Oncol 2022;13:59-68. [Crossref] [PubMed]
- Parpinel G, Laas-Faron E, Balaya V, et al. Survival after sentinel lymph node biopsy for early cervical cancers: a systematic review and meta-analysis. Int J Gynecol Cancer 2023;33:1853-60. [Crossref] [PubMed]
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Cervical Cancer (Version I 2018). National Comprehensive Cancer Network: Plymouth Meeting, PA, USA, 2017.
- Wang YZ, Deng L, Xu HC, et al. Laparoscopy versus laparotomy for the management of early stage cervical cancer. BMC Cancer 2015;15:928. [Crossref] [PubMed]
- Giannini A, D'Oria O, Bogani G, et al. Hysterectomy: Let's Step Up the Ladder of Evidence to Look Over the Horizon. J Clin Med 2022;11:6940. [Crossref] [PubMed]
- Ramirez PT, Frumovitz M, Pareja R, et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N Engl J Med 2018;379:1895-904. [Crossref] [PubMed]
- Bogani G, Di Donato V, Scambia G, et al. Radical Hysterectomy for Early Stage Cervical Cancer. Int J Environ Res Public Health 2022;19:11641. [Crossref] [PubMed]
- Alfonzo E, Wallin E, Ekdahl L, et al. No survival difference between robotic and open radical hysterectomy for women with early-stage cervical cancer: results from a nationwide population-based cohort study. Eur J Cancer 2019;116:169-77. [Crossref] [PubMed]
- Jin YM, Liu SS, Chen J, et al. Robotic radical hysterectomy is superior to laparoscopic radical hysterectomy and open radical hysterectomy in the treatment of cervical cancer. PLoS One 2018;13:e0193033. [Crossref] [PubMed]
- Long Y, Yao Y, Yao DS. Indocyanine green angiography for preserving the ureteral branch of the uterine artery during radical hysterectomy: Two case report. Medicine (Baltimore) 2018;97:e12692. [Crossref] [PubMed]
- Turnbull H, Burbos N, Abu-Freij M, et al. A novel approach to postoperative bladder care in women after radical hysterectomy. Arch Gynecol Obstet 2012;286:1007-10. [Crossref] [PubMed]
- Di Donato V, Bogani G, Casarin J, et al. Ten-year outcomes following laparoscopic and open abdominal radical hysterectomy for "low-risk" early-stage cervical cancer: A propensity-score based analysis. Gynecol Oncol 2023;174:49-54. [Crossref] [PubMed]
- Leitao MM Jr, Zhou QC, Brandt B, et al. The MEMORY Study: MulticentEr study of Minimally invasive surgery versus Open Radical hYsterectomy in the management of early-stage cervical cancer: Survival outcomes. Gynecol Oncol 2022;166:417-24. [Crossref] [PubMed]
- Bogani G, Donato VD, Scambia G, et al. Practice patterns and 90-day treatment-related morbidity in early-stage cervical cancer. Gynecol Oncol 2022;166:561-6. [Crossref] [PubMed]
- Bogani G, Cromi A, Serati M, et al. Predictors of postoperative morbidity after laparoscopic versus open radical hysterectomy plus external beam radiotherapy: a propensity-matched comparison. J Surg Oncol 2014;110:893-8. [Crossref] [PubMed]
- Lewicki PJ, Basourakos SP, Qiu Y, et al. Effect of a Randomized, Controlled Trial on Surgery for Cervical Cancer. N Engl J Med 2021;384:1669-71. [Crossref] [PubMed]
- Falconer H, Palsdottir K, Stalberg K, et al. Robot-assisted approach to cervical cancer (RACC): an international multi-center, open-label randomized controlled trial. Int J Gynecol Cancer 2019;29:1072-6. [Crossref] [PubMed]
- Capozzi VA, Monfardini L, Scarpelli E, et al. Urologic Complication after Laparoscopic Hysterectomy in Gynecology Oncology: A Single-Center Analysis and Narrative Review of the Literature. Medicina (Kaunas) 2022;58:1869. [Crossref] [PubMed]
- Likic IS, Kadija S, Ladjevic NG, et al. Analysis of urologic complications after radical hysterectomy. Am J Obstet Gynecol 2008;199:644.e1-3. [Crossref] [PubMed]
- Fujii S, Takakura K, Matsumura N, et al. Precise anatomy of the vesico-uterine ligament for radical hysterectomy. Gynecol Oncol 2007;104:186-91. [Crossref] [PubMed]
- Pikaart DP, Holloway RW, Ahmad S, et al. Clinical-pathologic and morbidity analyses of Types 2 and 3 abdominal radical hysterectomy for cervical cancer. Gynecol Oncol 2007;107:205-10. [Crossref] [PubMed]
- Cai HB, Chen HZ, Zhang F, et al. Clinical report of the modified Piver class III hysterectomy on invasive cervical cancer. Zhonghua Fu Chan Ke Za Zhi 2010;45:511-4. [PubMed]
- Yang X, Wang J, Wang Y, et al. Surgical Technique Based on Space Anatomy for Laparoscopic Radical Trachelectomy with Uterine Artery Preservation. J Laparoendosc Adv Surg Tech A 2021;31:705-9. [Crossref] [PubMed]
Cite this article as: Xie C, Luo J, Lin Y. Surgical technique of robotic Piver class III hysterectomy with preserving ureteral branch of uterine artery on early-stage invasive cervical cancer. Gynecol Pelvic Med 2023;6:26.


