A nearly scarless single-port laparoscopic lateral suspension surgery using “homemade” mesh: a surgical technique
Highlight box
Surgical Highlights
• It is a nearly scarless single-port laparoscopic lateral suspension surgery. Using “homemade” mesh eases the patients’ financial burden.
What is conventional and what is modified?
• Conventional laparoscopic lateral suspension (LLS) surgery uses three or four ports in the abdominal wall, and for suspension, a Manhes-type 5 mm forceps is used to create a retroperitoneal tunnel, which leaves several 5 to 10 mm postoperative scars. The mesh usually used is a TiLOOP® “Cross-shape” mesh which costs 18k RMB.
• In the improved surgical technique, the surgery was performed in a single-port laparoscopic approach, and a 2 mm puncture clamp replaced the 5 mm forceps. Moreover, we make a “homemade cross-shape” mesh from a standard 15 cm × 10 cm rectangle mesh which costs 6k RMB.
What is the implication, and what should change now?
• This improved surgical technique is a boon for young women who love beauty, and it reduces the cost of surgery.
Introduction
Background
Pelvic organ prolapse (POP) is a common and benign condition that affects millions of females. Many women with POP are asymptomatic. Some may present with bothersome symptoms, such as vaginal bulge or pressure, or with associated symptoms including urinary, defecatory or sexual dysfunction, which may adversely affect the quality of life and represent an indication for surgery. In a cohort study of 3,515 women undergoing surgery for POP, health-related quality of life in 7 out of 10 (70%) patients were improved over a 2-year follow-up period, and patient satisfaction was high (1). For the correction of POP, there are various surgical techniques described in the literature. Compared to laparoscopic sacrocolpopexy (LSCP), which is considered the gold standard in POP treatment, the advantage of laparoscopic lateral suspension (LLS) is that it avoids dissection at the promontory and the associated risks of serious neurological, vascular, or ureteral injuries, which are commonly reported in obese women and when anatomic variations exist (2). A study of 417 women with POP suggests that surgical correction of POP with LLS is a feasible alternative to LSCP and can be performed after hysterectomy (3). Recently, LLS is increasingly being offered as a treatment intervention for POP women. Here, we aim to introduce an improved LLS surgery which is less invasive and more cost-effective. One of the patients who underwent this improved LLS surgery was used as an example to illustrate this technique. The patient was admitted to our hospital with acute urinary retention, vaginal bulge, and daily discomfort, and she was diagnosed with uterine prolapse (POP-Q stage III), the anterior vaginal wall prolapse (POP-Q stage III), the posterior vaginal wall prolapse (POP-Q stage II), and urinary retention. The results of laboratory examinations were normal. The ultrasound of the pelvic floor indicated an enlarged posterior bladder angle of about 130° and severe uterine prolapse after the maximum Valsalva. Rectal prolapse was not observed in the resting state or after maximum Valsalva. A bladder catheter was left in place for relief of acute urinary retention. Because the patient was very concerned about the surgical scars and had financial constraints, we performed this improved LLS surgery on the patient. The POP-Q scores before and one year after the surgery are presented in Table 1. The patient was very satisfied with the result.
Table 1
| POP-Q system | Prior surgery | 1 year after surgery |
|---|---|---|
| POP-Q point Aa | −1 | −3 |
| POP-Q point Ba | +3 | −3 |
| POP-Q point C | +3 | −6 |
| POP-Q point Ap | −3 | −3 |
| POP-Q point Bp | +1 | −3 |
| POP-Q point D | +1 | −6 |
| TVL | 7 | 7 |
POP-Q, Pelvic Organ Prolapse Quantification System; TVL, total vaginal length.
Rationale
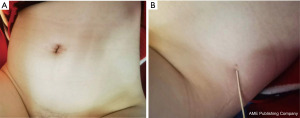
Conventional LLS surgery routinely uses 3 or 4 ports in the abdominal wall, and for suspension, from ‘outside-in’, a Manhes-type 5 mm forceps is used to create a retroperitoneal tunnel, which leaves several 5 to 10 mm postoperative scars on the abdomen by the forceps and trocar sites. It increases postoperative pain without any cosmetic effects. Postoperative scar cosmesis is a critical issue for women, especially for hyperplastic scars and young women. Surgeons are concerned about how to reduce the number of incisions and trocars. Recently, single-port laparoscopy was carried out to maximize the advantages of laparoscopic surgery, by reducing number of incisions and trocars (4). It has increased exponentially in popularity in gynecological surgery in the last decade. In our gynecology department, over 90% (about 3,000 cases) of gynecological surgeries have been performed in single port laparoscopic approach in the past 3 years. Increasing surgical experience made it possible to complete LLS in a single-port laparoscopic approach which left a nearly normal-looking umbilicus postoperatively. In the improved LLS surgery, a 2 mm puncture clamp replaces the 5 mm forceps to create a retroperitoneal tunnel, which leaves only two 1 mm postoperative scars on the abdomen (Figure 1) as we reported before (5). Furthermore, lateral attachment is provided by retroperitoneal fibrosis over the side arms postoperatively. It is very important not to widen the retroperitoneal tunnel diameter to avoid any risk of secondary slip and recurrence of the POP.
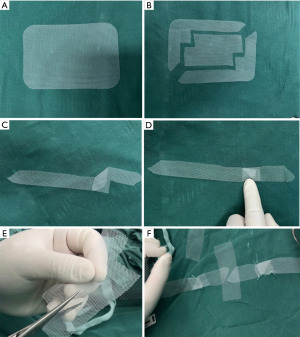
POP is more common in women living in rural areas with multiple deliveries. In China, the cost of mesh usually used in LLS surgery accounts for about 1/2 of all surgical costs, and the insurance does not cover the mesh. Most patients cannot afford it. Reducing the cost of the mesh could help these patients get better care. We use a standard 15 cm × 10 cm rectangle mesh to make a “homemade cross-shape” mesh (Figure 2), which reduces the mesh cost from 18k to 6k RMB.
Objective
We aim to introduce an improved LLS surgery that is less invasive and more cost-effective with almost invisible scars. We present this article in accordance with the SUPER reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-2/rc).
Preoperative preparations and requirements
Surgical contraindications needed to be excluded. Preoperative cervical cytological examination and diagnostic uterine curettage were performed to exclude malignant diseases if necessary.
Ethics approval was obtained from the Ethics Committee of Chengdu First People’s Hospital (No. 2022 XJS NO019). All procedures performed in this study were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this study and any accompanying images or video. A copy of the written consent is available for review by the editorial office of this journal.
Step-by-step description
After intubation, the patient was placed in a cystolithotomy position with the buttocks higher than the head. After a 2.5 cm longitudinal incision was made at the umbilicus, subcutaneous tissue and anterior abdominal fascia were incised layer by layer, then the peritoneum was incised. The disposable incision protection sleeve was placed in the incision, and pneumoperitoneum was then achieved by using the closed method with a multichannel port. The total hysterectomy with bilateral salpingectomy was successfully performed under standard surgical procedures which shown in the Video 1.
The method of making the “homemade” mesh is shown in Figure 2. Divided the standard 15 cm × 10 cm rectangle mesh (Figure 2A) into 3 parts (Figure 2B). Folded the “L-shape” mesh into an “I-shape” to make a 2 cm wide and 19 cm long tape (Figure 2C,2D), then sutured the fold site. The rest of the mesh was cut into a 3 cm wide and 6 cm long rectangle mesh (Figure 2E). Spliced the prepared cut-mesh into a “cross-shape” mesh and sutured the joints with non-absorbable suture material (Figure 2F).
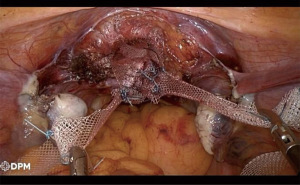
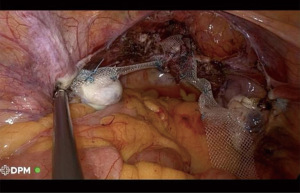
Placed the prepared “cross-shape” mesh into the abdominal cavity (Figure 3). Punctured the abdominal wall (located 4 cm posterior to the anterior superior iliac spine, 2 cm above the iliac crest) with a 2 mm needle. A 2 mm puncture clamp slid under the peritoneum, above the external iliac artery, until drilling out the round ligament. Grasped the mesh arms on both sides and pulled backward through the formed tunnel.
The arms of our “homemade” mesh were composed by folding and fixing an integral part of the mesh rather than cutting and reassembling, which avoided reducing the tensile strength of the mesh arms and fracturing at the joint especially after the suture degrading in the future. Furthermore, we optimized the design so that only one folded part was on the mesh arm and located at 4 cm away from the starting part. In the LLS surgery, this thickened folded part would be located at the edge of the round ligament and not enter the narrow tunnel made by the mere 2 mm clamp (Figure 4). So, the resistance of the mesh through the tunnel would not be increased and the potential damage to the vessel and muscle could be avoided. The starting part of the two arms mesh was sewn together with the rectangle mesh, then they were sutured to the vaginal wall, which reinforced the stability of the joints.
Postoperative considerations and tasks
Antibiotics were given within 48 hours after surgery to prevent infection. The patient had normal spontaneous urination after the catheter was removed 3 days after the surgery. Six months after the surgery, heavy physical activity should be avoided, stool should be kept unobstructed, and chronic cough should be actively treated. Long-term follow-up was required at least two years after the surgery.
Discussion
Surgical highlights
In this improved surgical technique, we performed the surgery by single-port laparoscopy, punctured the abdominal wall with a 2 mm needle, and created a retroperitoneal tunnel with a 2 mm puncture clamp, these improvement measures made the postoperative scars nearly invisible. Furthermore, we made a “homemade cross-shape” mesh from a standard 15 cm × 10 cm rectangle mesh, that greatly reduced the economic burden of patients.
Strengths and limitations
We improve the traditional LLS surgery by using single-port laparoscopy and tiny punctures, that greatly reduce the patients’ trauma and increase cosmetic effects. We also design a “homemade” mesh to reduce the surgical cost. The “homemade” mesh has standardized production methods, which is easy to learn. It does not increase the operation time by making the “homemade” mesh generally before the operation.
The limitation of this surgical technique is it cannot solve posterior pelvic defects, but we find that LLS with a cross-mesh placed over the top of the vagina after hysterectomy can solve mild to moderate posterior pelvic prolapse to some extent. Mesh-related complications including exposure or extrusion also exist.
Up to now, we have already performed this improved LLS surgery on 30 symptomatic POP patients. One patient had a pelvic infection within one week after the surgery and was treated with antibiotic, and one patient had chronic pelvic pain. The complication of umbilical incisional hernia was not observed in our study.
Implications and actions recommended
This improved surgical technique not only improves the quality of life of POP patients effectually but also meets their beauty needs and reduces the cost of surgery. This technique appears to be the optimal treatment for POP patients who have complaints of postoperative scars or have financial constraints. This improved surgical technique provides an avenue for gynecologic surgeons due to its minimally invasive character.
Conclusions
This report aims to introduce an improved LLS with less invasiveness by altering the approach of both the laparoscopy and the lateral suspension, and more cost-effective by using “homemade” mesh. To narrow the retroperitoneal tunnel could avoid the risk of secondary slip and recurrence of the POP. From the perspective of health economics, our “homemade” mesh is highly practical and has been widely used in our department. This improved LLS surgery is worth promoting in developing countries.
Acknowledgments
The video was awarded the third prize in the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery).
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-2/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-2/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-2/coif). The series “Award-Winning Videos from the Third International Elite Gynecologic Surgery Competition (2022 Masters of Gynecologic Surgery)” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethics approval was obtained from the Ethics Committee of Chengdu First People’s Hospital (No. 2022 XJS NO019). All procedures performed in this study were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this study and any accompanying images or video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mattsson NK, Karjalainen PK, Tolppanen AM, et al. Pelvic organ prolapse surgery and quality of life-a nationwide cohort study. Am J Obstet Gynecol 2020;222:588.e1-588.e10. [Crossref] [PubMed]
- Matthews CA. Minimally Invasive Sacrocolpopexy: How to Avoid Short- and Long-Term Complications. Curr Urol Rep 2016;17:81. [Crossref] [PubMed]
- Veit-Rubin N, Dubuisson JB, Gayet-Ageron A, et al. Patient satisfaction after laparoscopic lateral suspension with mesh for pelvic organ prolapse: outcome report of a continuous series of 417 patients. Int Urogynecol J 2017;28:1685-93. [Crossref] [PubMed]
- Choi YS, Park JN, Oh YS, et al. Single-port vs. conventional multi-port access laparoscopy-assisted vaginal hysterectomy: comparison of surgical outcomes and complications. Eur J Obstet Gynecol Reprod Biol 2013;169:366-9. [Crossref] [PubMed]
- Mao M, Xu N, Li YH, et al. A nearly scarless single-port laparoscopic lateral mesh suspension surgery. Asian J Surg 2023;46:5161-2. [Crossref] [PubMed]
Cite this article as: Xu N, Mao M, Li YH. A nearly scarless single-port laparoscopic lateral suspension surgery using “homemade” mesh: a surgical technique. Gynecol Pelvic Med 2023;6:27.