
Management of thrombosed urethral prolapse in a premenopausal adult woman: case report and literature review
Highlight box
Key findings
• We present a rare case of a thrombosed urethral prolapse in a premenopausal, adult woman and describe risk factors for her presentation and management of her condition.
What is known and what is new?
• Urethral prolapse is a rare occurrence, particularly in premenopausal, adult woman.
• The ideal management strategy of symptomatic urethral prolapse is unknown; however, it is reasonable to offer surgical excision for patients who have failed medical management, as it typically has excellent outcomes.
What is the implication, and what should change now?
• A review of potential conditions and medications causing a prolonged hypoestrogenic state or increased intra-abdominal pressure should be considered in premenopausal adult women presenting with urethral prolapse.
Introduction
Urethral prolapse is an infrequent lesion of the urethral meatus, whereby the urethral mucosa becomes circumferentially everted in a doughnut-shaped fashion. Over 80% of urethral prolapse cases are diagnosed in pre-pubertal girls, with the remaining occurring in adult women, generally of postmenopausal status (1). The condition is exceedingly rare, especially in premenopausal females. Acquired urethral prolapse is poorly understood and presumed to be due to several potential causes including separation of the longitudinal and circular smooth muscle layers of the urethra (congenital or traumatic), atrophy of the urethral meatus related to hypoestrogenism, chronic irritation, birth trauma, and increased intra-abdominal pressure (2,3).
Very few cases of urethral prolapse have been described in premenopausal, adult women. In this case report, we describe a case of a thrombosed and necrotic urethral prolapse in a 34-year-old woman. Following this, we describe the existing published cases of urethral prolapse in this patient population, risk factors for urethral prolapse, and management strategies. We present this case in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-17/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
A nulliparous 34-year-old Caucasian woman presented to our emergency room overnight with an enlarging and increasingly painful vaginal mass. Nine days prior, she experienced initial symptoms of light bleeding, dysuria, and a lesion near the urethra. She presented at an outside facility and was diagnosed with a urethral caruncle, as the lesion was located at the posterior urethral meatus (Figure 1). She was prescribed vaginal estrogen cream to be used three times weekly. She had no significant medical history or previous abdominopelvic surgery. She did endorse a recent residential move with lifting of heavy boxes. She was sexually active and had used intramuscular medroxyprogesterone every 12 weeks for the past 2.5 years. After her initial presentation, she noted an increasing size of the urethral lesion with worsening pain and continued bleeding, as well as slowed urinary stream.
On physical exam, she was afebrile and hemodynamically stable. She was noted to have a 2 cm purplish, round, friable lesion from the urethra which was tender to palpation and not actively bleeding. She had normal bladder emptying. Her complete blood count was without leukocytosis or anemia. Her basic metabolic panel showed normal kidney function and no electrolyte abnormalities. Her urinalysis showed large blood and trace leukocyte esterase, and point-of-care pregnancy test was negative. Computed tomography pelvis with contrast revealed a nodular protrusion at the level of the external urethral meatus. Magnetic resonance imaging pelvis showed an expansile mass-like thickening of the distal urethra, which was T2 hyperintense and not cystic, measuring 1.7 cm × 1.7 cm × 1.2 cm. There was no involvement of surrounding structures nor any pelvic lymphadenopathy. The patient was admitted and noted to have worsening pain and difficulty with voiding over the next 12 hours with an increase in lesion size to 3 cm (Figure 2). She was therefore recommended surgical excision. The most likely cause of her condition was felt to be a necrotic urethral prolapse or caruncle. Less likely causes included urethral polyp, carcinoma, and condyloma. To confirm diagnosis, cystoscopy was recommended with a consideration for surgical excision or biopsy. Solid masses with enlarged pelvic lymph nodes or invasion into surrounding structures on imaging would be concerning for malignancy.
In the operating room, a foley catheter was placed and the urethral mass was noted to be circumferential, consistent with a thrombosed urethral prolapse (Figure 3A). Dilute lidocaine with epinephrine was injected along the edges of the urethral mass. Absorbable stay sutures were placed in all 4 quadrants of the urethra. Electrocautery and sharp dissection were used to excise the necrotic tissue. The edges were then oversewn with interrupted absorbable sutures with care taken to incorporate the urethral mucosa (Figure 3B). A cystoscopy was then performed revealing normal bladder mucosa, free-flowing urine from both ureteral orifices, and good coaptation of the urethral mucosa without any defect. A urinary catheter was kept in place for 7 days postoperatively to maintain urethral patency during healing. The patient was recommended to continue vaginal estrogen use postoperatively until complete incisional healing.
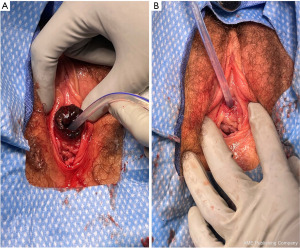
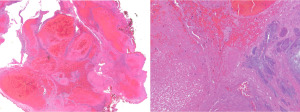
Although there was clinical concern for tissue necrosis, pathology showed granulation tissue with dilated and congested blood vessels, fibrin thrombus, and fibroinflammatory exudate without evidence of neoplasia or necrosis (Figure 4). The patient was seen at 2 weeks postoperatively with minimal pain and no voiding dysfunction. A 5-mm area of granulation tissue was noted and cauterized with silver nitrate. The patient was recommended to refrain from continued medroxyprogesterone usage and was counseled on alternative contraceptive options. At 10 weeks postoperatively, the patient had returned to her active lifestyle and was fully continent (Figure 5). She remains symptom-free without recurrence of urethral prolapse at one year.
Discussion
In the setting of a large, solitary urethral mass, it can be difficult to distinguish a urethral caruncle from urethral prolapse without first identifying the location of the urethral meatus, either with physical exam, insertion of a urinary catheter, or imaging (4). Moreover, urethral prolapse typically presents with non-specific urinary and vaginal symptoms which can delay diagnosis. Urethral caruncle is considered by some to be on the same spectrum as urethral prolapse (e.g., as a partial or single-quadrant prolapse) (5), while others define it to be a separate entity from prolapse (e.g., as a benign polypoid mass at the meatus compared to circumferential eversion of urethral mucosa) (6). Estrogen deficiency is a major risk factor for both urethral prolapse and caruncle, as it may lead to weakening of the periurethral fascia. A precipitating event that increases intra-abdominal pressure is more likely to be seen in urethral prolapse than urethral caruncle (1).
Urethral prolapse is exceedingly rare in premenopausal, adult woman. We postulate that our patient’s prolonged hypoestrogenic state caused by long-term intramuscular medroxyprogesterone and her recent heavy lifting while moving residencies were the main risk factors that led to urethral prolapse. The acute worsening of the urethral prolapse prior to surgical management was due to thrombosis of the prolapse and increasing edema, leading to difficulty with bladder emptying which caused the patient to strain, further worsening the swelling.
A review of the literature revealed that only six other cases of urethral prolapse in this patient population have been previously described (7-12). We will exclude one of these cases from the following discussion given the patient’s postmenopausal estrogenic state (38-year-old phenotypic female with 46XY karyotype and complete androgen insensitivity syndrome, who had undergone bilateral orchidectomy over 20 years prior) (7). The remaining five women were otherwise healthy with an age range of 18 to 46 years. They experienced symptoms (urethral mass, vaginal bleeding, and/or pain) over a period of 2 days to 7 years. Identified risk factors were recurrent increases of intra-abdominal pressure in two cases (e.g., due to farming occupation or lifting weights) and long-term (4 years) contraceptive use in one, while the other two cases did not identify any particular risk factor. Three of the five women were treated by surgical excision with excellent outcomes. One patient had successful treatment with local estrogen therapy and the other was prescribed an antibiotic for a urinary tract infection with consequent resolution of urethral prolapse. Of note, only one of the cases described necrosis and strangulation of the prolapse, necessitating more urgent management (11). Given the limited number of published cases in the literature, it may be difficult to draw conclusions on the importance of these risk factors and the safety of surgical management.
There is limited high-quality data on the management of urethral meatal lesions, and therefore practitioners must rely on expert opinion to guide treatment options. A systematic approach has been suggested by Maetzold and Takacs which distinguishes symptomatic and asymptomatic lesions (13). In the setting of symptomatic caruncles and prolapse, a 4–12-week trial of conservative management (topical estrogen, anti-inflammatory medications, and sitz baths) is recommended (10). Asymptomatic urethral caruncles and prolapse without features concerning for malignancy (e.g., solid mass, rapidly growth, ulceration, enlarged surrounding lymph nodes) do not require treatment. On the other hand, failure to improve with conservative management, acute urinary retention, thrombosis, and worsening pain are all indications for surgical excision. Lesions with malignant characteristics should also be biopsied or excised.
Notably, less than 10% of cases involving surgical excision of urethral prolapse and caruncles are performed due to thrombosis (5). Thrombosis of the prolapsed distal urethral tissue can lead to significant inflammation and edema which results in compression at the urethral meatus (14). This compromises vascularity and causes tissue necrosis, which necessitates urgent therapeutic intervention.
A common surgical approach is the “four-quadrant excisional technique” (15). Absorbable stay sutures are placed at the urethral lumen in all four quadrants and used for retraction as the mucosa tends to retract after excision of the prolapse. The edematous tissue is then excised quadrant-by-quadrant, with re-approximation of the mucosa to the surrounding epithelium after each quadrant is removed. Patients typically have favorable outcomes with surgical excision. An alternative to surgical excision is manual reduction of the prolapse, which has been performed successfully with the injection of lidocaine with hyaluronidase (16).
Overall, complication rates are low after surgical excision of thrombosed urethral prolapse. Complications include bleeding, urethral stenosis due to formation of scar tissue, urethral sphincter incompetence leading to stress urinary incontinence, and recurrence (2). Postoperatively, it is recommended that vaginal estrogen be continued to promote incisional healing for at least 6 weeks.
This case report adds to the limited literature on urethral prolapse in premenopausal adult women, as well as to the surgical outcome data on urethral prolapse excision. However, larger studies are required to better establish management strategies for urethral prolapse in this patient population. The narrative review in this case report provides patterns in presentation and care, but given the small number of cases included, is insufficient to alter current clinical practice.
Conclusions
A review of potential conditions and medications causing a prolonged hypoestrogenic state or increased intra-abdominal pressure should be considered in premenopausal adult women presenting with urethral prolapse. Restoration of estrogen to the urethra through the directed use of estrogen cream is the primary management of a symptomatic urethral caruncle or non-obstructive urethral prolapse. Surgical excision is a viable and safe option for symptomatic or thrombosed urethral prolapse. An indwelling urinary catheter is recommended upon discharge postoperatively. Postoperative follow-up should include an assessment of voiding dysfunction.
Patient perspective
“At first my mild symptoms felt similar to what a urinary tract infection feels like: the urge to urinate, slight discomfort in the area. When the symptoms did not progress as usual (I’ve had a few UTI’s), I grabbed a mirror to see if anything looked different in the area. I was shocked to find a red, round growth. Day by day, the lump grew in size and became much more painful. I was having bouts of extreme, sharp pain. It felt like I was trying to insert a tampon with glass shards attached to it. The pain took my breath away.
The mass was starting to become necrotic, [and] I underwent emergency surgery to have the mass removed. The surgery seemed to go well, and I woke up to the news that my urethra had prolapsed completely. My recovery went as planned and after a week at home with a catheter, I was able to return to a somewhat normal life. I abstained from sexual activity and swimming for a few months afterward to ensure I was healed. Overall, I am grateful for the care I received, especially by my surgeons and the nurses who advocated for my admissions and emergency surgery. I am surprised by how few people understood what was going on, but now I realize that this is not a typical issue. I am comforted that my experience might be able to help others or point them in a direction toward a care plan that makes sense for them.”
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-17/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-17/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-23-17/coif). S.W.Z. reported a Magee Womens Research Institute Restricted Fund Grant, Magee Womens Research Institute-Penn State Behrend SEED Grant and Wishwa N. Kapoor Catalyst Fund Grant. GSN reported grants or contracts from Magee-Womens Research Foundation, PFD Research Foundation, National Institute of Child Health and Human Development and National Heart, Lung, and Blood Institute. G.S.N. also reported payment from Brigham and Womens Hospital Grand Rounds and she serves in L’Ecole du Samedi. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hillyer S, Mooppan U, Kim H, et al. Diagnosis and treatment of urethral prolapse in children: experience with 34 cases. Urology 2009;73:1008-11. [Crossref] [PubMed]
- Hill AJ, Siff L, Vasavada SP, et al. Surgical excision of urethral prolapse. Int Urogynecol J 2016;27:1601-3. [Crossref] [PubMed]
- Jalloh M, Heibig J, Gaye O, et al. Urethral Prolapse Case Report: Surgical and Social Considerations in Senegal. Case Rep Urol 2022;2022:5541416. [Crossref] [PubMed]
- Abuhasanein S, Holmin E, Swärd J, et al. A rare case of a necrotized urethral prolapse in a postmenopausal woman with acute urinary retention. Low Urin Tract Symptoms 2021;13:505-8. [Crossref] [PubMed]
- Hall ME, Oyesanya T, Cameron AP. Results of surgical excision of urethral prolapse in symptomatic patients. Neurourol Urodyn 2017;36:2049-55. [Crossref] [PubMed]
- Meutia AP, Yonathan K, Widia F. Giant urethral caruncle resembling urethral prolapse causing outflow obstruction. Urol Case Rep 2021;39:101783. [Crossref] [PubMed]
- Watson H, Stasiowska E. A case report of urethral prolapse in a 38 year old female with 46XY karyotype. Arch Ital Urol Androl 2014;86:140-1. [Crossref] [PubMed]
- Eke N, Ugboma HA, Eke F. Urethral prolapse in a woman in her reproductive age--a very rare occurrence. Niger J Med 2005;14:431-3. [PubMed]
- Olumide A, Kayode Olusegun A, Babatola B. Urethral mucosa prolapse in an 18-year-old adolescent. Case Rep Obstet Gynecol 2013;2013:231709. [Crossref] [PubMed]
- Schreiner L, Nygaard CC, Anschau F. Urethral prolapse in premenopausal, healthy adult woman. Int Urogynecol J 2013;24:353-4. [Crossref] [PubMed]
- Jessop ML, Zaslau S, Al-Omar O. A Case of Strangulated Urethral Prolapse in a Premenopausal Adult Female. Case Rep Urol 2016;2016:1802623. [Crossref] [PubMed]
- Fornari A, Gressler M, Murari JCL. Urethral Prolapse: A Case Series and Literature Review. J Obstet Gynaecol India 2020;70:158-62. [Crossref] [PubMed]
- Maetzold E, Takacs EB. Urethral Pathology in Women. Curr Urol Rep 2022;23:225-34. [Crossref] [PubMed]
- Sharma A, Garg G, Singh BP, et al. Strangulated urethral prolapse in a postmenopausal woman presenting as acute urinary retention. BMJ Case Rep 2018;2018:bcr2018227040. [Crossref] [PubMed]
- Shurtleff BT, Barone JG. Urethral prolapse: four quadrant excisional technique. J Pediatr Adolesc Gynecol 2002;15:209-11. [Crossref] [PubMed]
- Ho KL, Chu SM, Tam PC. Reduction of strangulated urethral prolapse using local anesthesia with hyaluronidase. J Urol 2003;169:288. [Crossref] [PubMed]
Cite this article as: Zuo SW, Napoé GS. Management of thrombosed urethral prolapse in a premenopausal adult woman: case report and literature review. Gynecol Pelvic Med 2023;6:33.





