
Pneumovaginal endoscopic surgery to vaginal septum resection: a case report and literature review
Highlight box
Key findings
• Pneumovaginal endoscopic surgery provides a valuable alternative to conventional vaginal surgery for septum resections. This technique offers an improved view of the anatomic structures with greater exposure to the section plans and a more comfortable and ergonomic operating position, allowing for easy, safe, and precise resections.
What is known and what is new?
• Vaginal septal excisions can be performed via direct speculoscopy, using laparoscopic instruments through a speculum, or using hysteroscopic instruments. Report here about what does this manuscript adds.
• Pneumovaginal endoscopic surgery can be a valuable alternative to perform vaginal septal excisions.
What is the implication, and what should change now?
• Although conventional vaginal access could be a valid option to treat vaginal conditions in most patients, the pneumovaginal endoscopic approach could represent a useful alternative, especially in the case of difficult vaginal exposure.
Introduction
Background
A longitudinal vaginal septum results from an incomplete fusion of the Mullerian ducts and is often associated with uterine anomalies. Several types of longitudinal vaginal septa exist based on the degree of completeness of vaginal division (partial or complete), the symmetricity, the position (with left or right dominant side), the association with the cervix (merged or isolated forms), and concomitant vaginal openings (regular or narrow) (1). Longitudinal vaginal septa can cause dyspareunia, difficult tampon insertion, persistent vaginal bleeding despite tampon placement, and dysmenorrhea in the case of obstructed hemivagina. Surgical treatments can indicate improved symptoms and can generally include septal excisions through direct speculoscopy, using laparoscopic instruments through a speculum (without pneumovagina), or using hysteroscopic instruments (1). Pneumovaginal endoscopic surgery is a new surgical approach especially used to treat vaginal conditions such as erosions of synthetic mesh used for pelvic organ prolapse or vaginal leiomyoma. Here, we present a case of vaginal septal excision using a pneumovaginal endoscopic approach.
Rationale and knowledge gap
Since current knowledge regarding pneumovaginal endoscopic surgery is very limited and based on a small number of scientific reports, any additional evidence is useful to prove the feasibility and safety of this surgical approach. In addition, vaginal septal excision using pneumovaginal endoscopic surgery has been reported only once. Our case, in association with a literature review on all cases of vaginal conditions treated with this surgical approach, could help to increase scientific knowledge on this topic.
Objective
The aim of this study was to present a novel technique to perform vaginal septal excisions using pneumovaginal endoscopic surgery using original video footage and to report an updated literature review on all cases of vaginal conditions treated with this surgical approach. We present this case in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-46/rc).
Case presentation
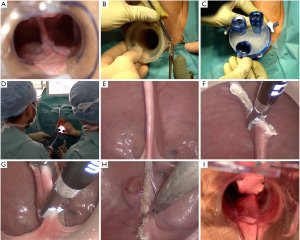
A 24-year-old nulliparous woman presented with chronic dyspareunia due to a longitudinal vaginal septum (Figure 1A) associated with uterocervical malformation type U3C2V1 according to the ESHRE/ESGE classification (2) (confirmed with magnetic resonance imaging). The septum appeared complete, symmetric, and merged with the space in between the cervices with a normal vaginal opening. On February 13, 2020, we performed a total septal excision using a pneumovaginal endoscopic approach. This surgical approach was chosen to overcome the problem posed by the deep and narrow vagina of this nulliparous patient, which made it difficult to access the deeper portion of the septum.
All procedures performed in this study were in accordance with the ethical standards of the national research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Surgical technique
The patient was placed in a dorsal lithotomy position under general anesthesia. Using a GelPOINT Path Transanal Access Platform (Applied Medical, Rancho Santa Margarita, CA, USA), a pneumovagina was created at a pressure of 6 mmHg (Figure 1B,1C). The surgeon and assistant were seated between the patient’s legs (Figure 1D). The vaginal septum and cervices were exposed (Figure 1E). The vaginal septum was resected using an endoscopic sealer/divider device cutting close to both the anterior (Figure 1F) and the posterior vaginal wall (Figure 1G). The resection line on the posterior vaginal wall was endoscopically sutured using a 2/0 absorbable thread to approach the margins and to reduce the risk of synechiae formation (Figure 1H). The intervention lasted 20 minutes, and we observed no intraoperative complications. This surgical technique is demonstrated in Video 1.
Postoperative follow-up
The patient was discharged the same day after surgery. She needed no postoperative medicaments. During the 6-month follow-up, the patient reported a rapid and complete resolution of dyspareunia without complications and with complete vaginal wall healing (Figure 1I).
Discussion
Key findings
We described a case of complete longitudinal vaginal septum treated using a pneumovaginal endoscopic approach. Our findings, in association with the reported literature review, suggest that this surgical technique is feasible and effective for treating some vaginal conditions, including vaginal septa.
Strengths and limitations
The main limitation of this study is that it is a single case report, and no conclusions can be drawn from this type of study. Nevertheless, our case, associated with the following literature review on all cases of vaginal conditions treated with pneumovaginal endoscopic surgery, could improve the knowledge on this topic.
Comparison with similar researches
Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) is an emerging minimally invasive approach used to treat several intrabdominal gynecological conditions (3). Similarly, we used an analogous approach to treat a condition limited to the vaginal cavity. Creating a pneumovagina with a single-port device allows laparoscopic techniques in performing some vaginal surgeries. This technique offers an improved view of the anatomic structures with greater exposure to the section plans and a more comfortable and ergonomic operating position. These characteristics are most important in the case of difficult access, such as for deep vaginas, tumors of the anterior wall, and a restricted vaginal canal, for which good surgical field exposure is often challenging.
We reviewed the English, French, Italian, and Spanish literature published on the PubMed database on all cases using pneumovaginal endoscopic approaches to treat vaginal conditions (Table 1) (4-11). Including our patient, there are 17 reported cases of pneumovaginal endoscopic surgery performed to treat vaginal erosions of synthetic mesh used for pelvic organ prolapse, vaginal septum, vaginal leiomyoma, and vaginal wall recurrences of uterine, cervical, and ovarian cancers. In addition, a similar approach could be used to access the Douglas pouch under continuous view to reduce the risk of iatrogenic pelvic organ damages during peritoneal cavity access in the case of vNOTES approaches for patients with suspected pelvic adhesions (12). Menopausal status and parity seem not to influence the feasibility of pneumovaginal endoscopic surgeries, with several reported cases of pre- and postmenopausal women, as well as nulliparous and multiparous women (4-11). To create a pneumovagina, three leading single-port platforms have been used; the SILS™ port (4,5), the GelPOINT® V-Path Transvaginal Access Platform (6,10), and the GelPOINT® Path Transanal Access Platform (7,9,11). Standard laparoscopic instruments and optics are used to perform the interventions, with the possibility of using electrosurgery instruments or performing endoscopic sutures. No intra- and postoperative complications have been observed, and patients recover rapidly after surgery. Although no case has been reported, as for vNOTES, pneumovaginal endoscopic surgery does not represent a contraindication to pregnancy and vaginal delivery (13). No specific risks or disadvantages seem to be associated with this surgical approach to vaginal septum resections. However, more studies are required to confirm its safety on a larger number of patients.
Table 1
| Reference | Study size (n) | Age (years) | Parity | Vaginal condition | Symptoms | Interventions | Surgical system | Operation time (min) | Complications | Discharge time |
|---|---|---|---|---|---|---|---|---|---|---|
| Billone et al., 2015 | 5 | – | – | Mesh erosion through the vagina as a complication of synthetic mesh used for pelvic organ prolapse repair | – | Mesh excision and vaginal wall repair | SILS™ port | – | No | The same day |
| Mohr et al., 2017 | 1 | 60 | – | Mesh erosion with abscess formation at vaginal apex 22 months after laparoscopic sacrocolpopexy | Foul-smelling discharge for 1 year | Mesh excision and abscess drainage | SILS™ port | – | No | – |
| Schaub et al., 2018 | 1 | 59 | – | Mesh erosion with abscess formation | Foul-smelling discharge | Mesh excision and abscess drainage | GelPOINT® V-Path Transvaginal Access Platform | 60 | No | – |
| Heredia et al., 2020 | 2 | 35 | – | Incomplete longitudinal septum in the proximal 2/3 of the vagina associated with bicornuate unicollis uterus | Dyspareunia | Complete septum resection | GelPOINT® Path Transanal Access Platform | 5 | No | 4 hours |
| 36 | Nulliparous | 3-cm leiomyoma in the proximal vaginal third | Dyspareunia | Myomectomy | GelPOINT® Path Transanal Access Platform | 35 | No | 12 hours | ||
| Liu et al., 2021 | 1 | 35 | Nulliparous | Leiomyoma in the proximal anterior vaginal wall (3.0 cm × 3.4 cm) | Asymptomatic | Myomectomy and vaginal wall repair | Transvaginal multichannel single-port | 20 | No | 5 hours |
| Kita et al., 2021 | 1 | 39 | Nulliparous | Left vaginal wall recurrence of an ovarian granulosa cell tumor (3.5 cm), 23 years after primary surgery | – | Tumor resection | GelPOINT® Path Transanal Access Platform | 88 | No | 3 days |
| Allary et al., 2021 | 1 | 42 | 2 | 4-cm leiomyoma in the posterior vaginal wall | Chronic pelvic pain | Myomectomy and vaginal wall repair | GelPOINT® V-Path Transvaginal Access Platform | – | No | 1 day |
| Yokoe et al., 2023 | 4 | 74 | – | Vaginal wall recurrence of an endometrial cancer | None | Tumor resection* | GelPOINT® Path Transanal Access Platform | 218 | No | – |
| 53 | – | Vaginal wall recurrence of a cervical cancer | None | Tumor resection* | GelPOINT® Path Transanal Access Platform | 292 | No | – | ||
| 51 | – | Vaginal wall recurrence of an ovarian cancer | Genital bleeding | Tumor resection* | GelPOINT® Path Transanal Access Platform | 121 | No | – | ||
| 79 | – | Vaginal wall recurrence of an endometrial cancer | Genital bleeding | Tumor resection* | GelPOINT® Path Transanal Access Platform | 165 | No | – | ||
| Our case | 1 | 24 | Nulliparous | Complete longitudinal vaginal septum associated with bicornuate bicollis uterus | Dyspareunia | Complete septum resection and vaginal wall repair | GelPOINT® Path Transanal Access Platform | 20 | No | The same day |
–: not reported. *, bi-directional approach (laparoscopic and vaginoscopic).
Explanations of findings
These results suggest that pneumovaginal endoscopic surgery is a feasible and safe approach to treating some vaginal conditions, with rapid recovery and no specific short- and long-term complications. In our case, we obtained easy access and exposure to the vaginal cavity, with favorable conditions to perform septal resection and endoscopic sutures. Although conventional vaginal access could be a valid option to treat vaginal conditions in most patients, this pneumovaginal endoscopic approach could represent a useful alternative in the case of difficult vaginal exposure (e.g., obesity, narrow vaginal canal, deep vagina).
Implications and actions needed
This study suggests the feasibility of using pneumovaginal endoscopic surgery to treating some vaginal conditions, including vaginal septum. However, before expanding this approach outside study settings, strong evidence of its feasibility, practical benefits, and long-term outcomes are needed.
Conclusions
We conclude that pneumovaginal endoscopic surgery could be a valid alternative to the conventional approach to treat some vaginal conditions. This approach appears safe and feasible. Nevertheless, these data come from case reports or small case series, and further studies are needed to evaluate this approach’s safety and indications in a more significant number of patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-46/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-46/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-22-46/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the national research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ludwin A, Lindheim SR, Bhagavath B, et al. Longitudinal vaginal septum: a proposed classification and surgical management. Fertil Steril 2020;114:899-901. [Crossref] [PubMed]
- Grimbizis GF, Gordts S, Di Spiezio Sardo A, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod 2013;28:2032-44. [Crossref] [PubMed]
- Li CB, Hua KQ. Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecologic surgeries: A systematic review. Asian J Surg 2020;43:44-51. [Crossref] [PubMed]
- Billone V, Amorim-Costa C, Campos S, et al. Laparoscopy-like operative vaginoscopy: a new approach to manage mesh erosions. J Minim Invasive Gynecol 2015;22:10. [Crossref] [PubMed]
- Mohr S, Siegenthaler F, Imboden S, et al. Transvaginal Excision of an Eroded Sacrocolpopexy Mesh by Using Single-Incision Laparoscopic Surgery Equipment. J Minim Invasive Gynecol 2017;24:1079-80. [Crossref] [PubMed]
- Schaub M, Lecointre L, Faller E, et al. Transvaginal Resection of an Infected Sacrocolpopexy Mesh by Single-Port Trocar. J Minim Invasive Gynecol 2018;25:391-2. [Crossref] [PubMed]
- Heredia F, Donetch G, Escalona J, et al. Single-Port/Pneumovagina Technique for Two Further Applications. J Minim Invasive Gynecol 2020;27:807-8. [Crossref] [PubMed]
- Liu JH, Zheng Y, Wang YW. Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) as treatment for upper vaginal leiomyoma: A case report. Medicine (Baltimore) 2021;100:e25969. [Crossref] [PubMed]
- Kita M, Sumi G, Butsuhara Y, et al. Resection of vaginal recurrence of granulosa cell tumor by pneumovaginal endoscopic surgery. Gynecol Oncol Rep 2021;36:100743. [Crossref] [PubMed]
- Allary M, Agostini A, Calderon L, et al. Using pneumovaginoscopy to perform the removal of a vaginal fibroid. Fertil Steril 2021;116:1664-6. [Crossref] [PubMed]
- Yokoe T, Kita M, Butsuhara Y, et al. R0 resection of vaginal stump recurrence of gynecologic malignancy by bi-directional endoscopic approach: A case series of four patients. Asian J Endosc Surg 2023;16:82-5. [Crossref] [PubMed]
- Hurni Y, Romito F, Huber DE. Is transvaginal natural orifice transluminal endoscopic surgery (vNOTES) indicated in patients with previous extensive pelvic surgeries? A case report. Case Rep Womens Health 2022;34:e00397. [Crossref] [PubMed]
- Tavano I, Housmans S, Bosteels J, et al. Pregnancy Outcome after Vaginal Natural Orifice Transluminal Endoscopic Surgery, a First Retrospective Observational Cohort Study. Gynecol Obstet Invest 2021;86:432-7. [Crossref] [PubMed]
Cite this article as: Shabanov S, Hurni Y, Lopes A, Brossard P. Pneumovaginal endoscopic surgery to vaginal septum resection: a case report and literature review. Gynecol Pelvic Med 2023;6:10.


