
Mini-sling Ophira in treatment of stress urinary incontinence: experience of the Urology Clinic of A.I. Yevdokimov Moscow State University of Medicine and Dentistry
Introduction
The surgical treatment of urinary incontinence has undergone significant changes over the past two decades. The development of the theory of the pathogenesis of urinary incontinence and the subsequent appearance of the TVT surgery was a true revolutionary event in urology (1). The main disadvantage of TVT surgery is the need for cystoscopy, blind conduction and, therefore, a high risk of bladder perforation (2). Performing TVT-O and TOT operations, where transobturator approach is used, is sometimes complicated by damage to the obturator nerve, followed by the development of chronic groin pain syndrome (3). The process of further improvement of the technique of sling surgery has led to the emergence of a new generation of synthetic slings. We are talking about “single-incision mini-sling”.
Mini-slings are in many ways derived from existing synthetic slings. The main difference from full-size sling is the method of their placement and, accordingly, the design features. Mini-slings are not delivered on the skin, but buried, where they are reliably fixed with special attachments.
In a relatively short period of time, mini-slings have managed to occupy a certain channel among the methods of surgical treatment of stress urinary incontinence. This study evaluates the effectiveness of the most commonly used mini-sling Ophira in our practice.
We present the following article in accordance with the STROBE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-22/rc).
Methods
In our urology clinic Ophira has been performed since 2010. The present study included patients who underwent this surgical intervention in the period from February 2010 to July 2012. A total of 68 patients took part in the study.
The average age of the patients was 58.7 years (31–85 years). Most of the patients were upward 45 years old. Only 3 patients (4.4%) were younger than the defined age. All patients had at least 1 parity in the anamnesis.
Medical history and physical examination with obligatory cough test were performed in all patients. The study included patients who did not have pelvic organ prolapse or the degree of prolapse was minimal.
Stress urinary incontinence was diagnosed in 60 patients (88.4%). Eight patients (11.6%) had a combined form of urinary incontinence with predominance of the stress component. In 10 patients (14.7%), stress urinary incontinence developed after previous surgical treatment of pelvic organ prolapse. In 3 patients (4.4%), there was a recurrent form of urinary incontinence after previous sling surgery. One patient (1.5%) had a history of a pelvic fracture with a violation of the integrity of the pelvic ring.
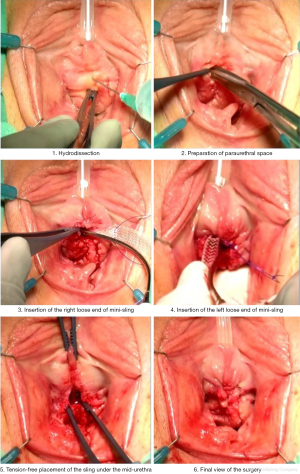
Ophira surgery was performed according to standard techniques. The main stages of the surgical operation are shown in Figure 1.
In 55 patients (80.9%), Ophira surgery was performed under spinal anesthesia. In 13 patients (19.1%), this surgery treatment was performed under local anesthesia. After surgery, all patients were determined by residual urine volume using ultrasound examination (US). The maximum permissible residual urine volume was 100 mL.
All patients were invited for follow-up: 1 month and 1 year after surgery. In all cases, physical examination was performed with cough test, uroflowmetry, as well as measurement of residual urine volume. The criterion for the effectiveness of the performed surgery was negative cough test, with absence or presence less than 100 mL of residual urine.
All patients were questioned about their satisfaction with the performed surgery. 5-point analogue scale was used: 1—very bad; 2—bad, 3—moderate, 4—good; 5—excellent.
The study was conducted following the Declaration of Helsinki (as revised in 2013). The study was approved by the local ethics committee of A.I. Yevdokimov Moscow State University of Medicine and Dentistry (No.: 06001604) and informed consent was taken from all individual participants.
Statistical analysis
This was a descriptive study and standard statistical analyses were performed. Statistical analysis was performed with the aid of Statistic XL v 1.8 and SISA. P values <0.05 were considered as statistically significant. Numerical variables were compared between groups by Mann-Whitney’s u-test and for paired comparisons the paired t-test were used.
Results
We have not encountered any major intraoperative complications. Only in one case there was blood loss more than 100 mL. After removal of the catheter, 4 patients (5.9%) had difficult urination and residual urine volume more than 100 mL. However, against the background of stimulating therapy, clinically significant effect was achieved in 3 cases. In 1 patient, despite the treatment, a significant volume of residual urine remained, which required cutting the loop.
All 68 patients were examined 1 month after surgery. A negative cough test was recorded in 58 patients (85.3%). A positive cough test was observed in 10 patients (14.7%). 59 patients (86.8%) had no residual urine. Residual urine was detected in 5 patients (7.4%), but its volume in all cases was less than 100 mL. 3 patients (4.4%) reported pain after surgery. In 5 patients (7.4%), signs of bladder hyperactivity appeared.
Regarding subjective assessment of the surgery, 49 patients (72.1%) were pleased with the result of the surgery (“4—good” and “5—excellent” on the visual analogue scale). 13 patients (19.1%) were satisfied with the results of the surgery (“3—satisfactory”). 6 patients (8.8%) were dissatisfied with the results of treatment (indicators “2—bad” and “1—very bad”).
Sixty-three patients (92.6%) were examined 12 months after the surgery. In our clinic, the follow-up was not performed in 5 patients (7.4%), for various reasons. A negative cough test was observed in 55 patients (87.3%). In 8 patients (12.3%) cough test was positive. We did not record any recurrence of urinary incontinence. Two patients (3.2%) had a residual urine volume less than 100 mL. Two patients (3.2%) had signs of overactive bladder. 1 patient (1.6%) still had pain. 50 patients (79.4%) are pleased with the result of the surgery. 9 patients are satisfied with the treatment results (14.3%). 4 patients (6.3%) were dissatisfied with the treatment results.
Discussion
One of the features of mini-sling Ophira is the design of the self-fixating tips. They are designed like a “harpoon” or “fishbone”, but unlike other mini-slings, they have several fixation points, which provides a more reliable attachment in muscle tissue. Loop implantation is performed using a special guide trocar, which allows you to control the process of implantation and its tension. Also, the design of the loop allows you to reduce excessive compression of the urethra at any stage of the surgery intervention.
Despite the fact that mini-slings have been used in clinical practice since 2006, the number of publications on this topic remains rather low. In one of them, the degree of fixation of various loops in tissues in experiments on mice is assessed (4). As shown by the results of the study, mini-sling Ophira loop has the best tissue fixation.
In another work by the same author, the experience of using the mini-sling Ophira in 124 patients was presented (5). Twelve months after the surgery, 81 patients (85.3%) had complete urinary continence, while improvement was observed in 6 patients (6.3%). Recurrence of urinary incontinence was observed in 8 patients (8.4%).
In 2011, Abdel-Fattah published meta-analysis of studies evaluating the effectiveness of mini-slings (6). A total of 758 patients were included in the study review. The average follow-up was 9.5 months. The authors of review described that the subjective and objective effectiveness of mini-slings is lower than standard sling surgery (RR: 0.83; 95% CI: 0.70–0.99, and RR: 0.85; 95% CI: 0.74–0.97, respectively). No significant differences were found in the incidence of intra- and postoperative complications.
When discussing the results of using any mini-sling, it is necessary to answer the question about role of this group of slings in clinical practice. In general, the question, what specific loop is indicated to the patient, is the most difficult in modern urogynecology. At this time, there are no clear indications for performing mini-sling surgery in modern literature. Our study included patients with various types of urinary incontinence, including recurrent forms.
In the case of mixed form of urinary incontinence, combined urodynamic study is very important, as well as clinical interview. In our opinion, patients with combined form of urinary incontinence can be operated on if the patient’s main complaint is involuntary leakage of urine during exertion, coughing, sneezing (when the stress component predominates). In the case of the prevalence of urinary urgency, it is more appropriate to start treatment with the elimination of the overactive bladder.
The experience of the surgeon is very important. In our experience, there is learning curve for mini-slings. Table 1 presents data on the number of complications observed by us for the entire time of this surgery intervention. We divided the group of patients into 4 subgroups, arranging them in chronological order. As you can see, the majority of complications occurred at the initial stages of adoption of approach. It should be noted that at the time of the beginning of the use of mini-slings in our practice, we already had quite significant experience in sling surgery. Nevertheless, this circumstance did not save us from the stage of adoption of approach.
Table 1
| Patients in order of performing | 1–14 | 15–30 | 31–45 | 46–68 |
|---|---|---|---|---|
| Complications | 4 | 2 | 1 | 0 |
| Successful treatment (negative cough test) | 71.4% | 85.7% | 92.8% | 93.7% |
Patients are divided according to the chronological order of their intervention. The more experience surgeon gets, the fewer complications are met.
In our opinion, the main mistakes leading to a negative result are incorrect positioning of the loop (for example, positioning under the proximal third of the urethra) and excessive tension. Therefore, specialists wishing to study this type of surgery should be trained in specialized training centers.
The choice of anesthesia is important. We considered implantation of mini-sling Ophira under local anesthesia. The choice of the method of anesthesia should be performed with the participation of the anesthesiologist and the patient herself. In the case of choosing regional anesthesia, it is necessary to conduct counseling interview with the patient before the surgical intervention, to tell her about surgical stages, as well as what sensations she may experience.
It should be noted that regional anesthesia, in our opinion, has number of undeniable advantages. The main difficulty associated with positioning any modern synthetic loop is controlling the degree of tension. In the modern literature, there is no data on the successful application of any objective method of loop tension control. Most experts agree that the personal experience of each surgeon plays a key role in this issue.
Continuing the topic of indications for performing the Ophira surgery procedures, it should be noted that this sling can be implanted in patients with recurrent urinary incontinence after previous sling surgeries, where obturator or retropubic route was used. Despite the fact that we have little experience of treating patients with recurrent urinary incontinence using mini-sling Ophira, the available data indicate the possibility of performing this surgery intervention in this group of patients.
A negative assessment of the results of the surgery by the patient is usually due to the development of various postoperative complications. Symptoms of overactive bladder, difficult urination, pain can significantly affect the patient’s perception of the outcome of the operation. In this regard, it is necessary to inform the patient about the probability of success, as well as about the possible complications of surgical treatment.
In conclusion, it should be noted that with the right choice of patients for this operation, adequate preoperative assessment and planning, as well as strict adherence to the stages of the operation, mini-sling Ophira provides a sufficiently high efficiency and a small number of complications in the surgical treatment of stress urinary incontinence.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Alexander Popov) for the series “Surgical Treatment of Genital Prolapse and Urinary Incontinence” published in Gynecology and Pelvic Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-22/rc
Data Sharing Statement: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-22/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-22/coif). The series “Surgical Treatment of Genital Prolapse and Urinary Incontinence” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted following the Declaration of Helsinki (as revised in 2013). The study was approved by the local ethics committee of A.I. Yevdokimov Moscow State University of Medicine and Dentistry (No.: 06001604) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ulmsten U, Henriksson L, Johnson P, et al. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 1996;7:81-5; discussion 85-6. [Crossref] [PubMed]
- Kuuva N, Nilsson CG. A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand 2002;81:72-7. [Crossref] [PubMed]
- Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 2009;CD006375. [PubMed]
- Palma P, Siniscalchi RT, Maciel LC, et al. Primary fixation of mini slings: a comparative biomechanical study in vivo. Int Braz J Urol 2012;38:258-65; discussion 265-6. [Crossref] [PubMed]
- Palma P, Riccetto C, Bronzatto E. Efficacy of ophira mini sling system for stress urinary incontinence: mid-term follow up of 124 patients in a multicentre international clinical trial. Available online: https://www.ics.org/Abstracts/Publish/134/000591.pdf
- Abdel-Fattah M, Ford JA, Lim CP, et al. Single-incision mini-slings versus standard midurethral slings in surgical management of female stress urinary incontinence: a meta-analysis of effectiveness and complications. Eur Urol 2011;60:468-80. [Crossref] [PubMed]
Cite this article as: Gvozdev M, Dzhuraeva M, Arefyeva O, Pushkar D. Mini-sling Ophira in treatment of stress urinary incontinence: experience of the Urology Clinic of A.I. Yevdokimov Moscow State University of Medicine and Dentistry. Gynecol Pelvic Med 2022;5:4.


