
Gastric cancer in a 22-year-old woman with metastasis to the cervix: a case report and literature review
Introduction
Ovarian metastases caused by gastric cancer, known as Krukenberg’s tumor, occur occasionally, but cervical metastases are rare. It has been speculated that the reasons for cervical metastasis include small tumor volume, low blood flow, distal circulation and rich fibrous tissue content. We present a rare case of advanced gastric cancer with metastasis to the cervix and primary presentation of vaginal bleeding. To our knowledge, this is the youngest patient identified to date.
We present the following case in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-32/rc).
Case presentation
A 22-year-old woman (0 gravida, 0 para) was referred to hospital in Shanghai on July 26, 2019 with a 2-month history of menstrual dysregulation and genital bleeding following intercourse. Gynecological examination revealed moderate erosion of the cervix with contact bleeding. Vaginal B-ultrasound showed that the size of the right ovary was 27×29×20 mm, and the internal echoless area was 20×19×17 mm. No abnormalities were found upon cervical liquid-based cytology or human papilloma virus (HPV) typing. She was diagnosed. She returned to hospital in October 2019 because her symptoms had not improved significantly after treatment. Vaginal B‑ultrasonography revealed a 2.8×1.4×2.8 cm cystic space on the right ovary, and the cystic fluid was not clear. The size of the left ovary was 3.8×1.6×1.7 cm, with multiple follicles (more than 12 in one section). She was referred for female hormone tests which showed the following: E2: 27.5 pg/mL, P: 0.88 ng/mL, T: 0.4 ng/mL, LH: 4.7 IU/L, FSH: 4.9 IU/L, PRL: 18.6 ng/mL. The initial diagnosis was polycystic ovary syndrome, for which she was advised to continue oral Diane-35 treatment.
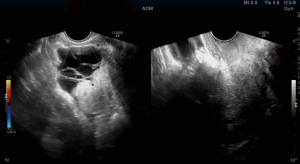
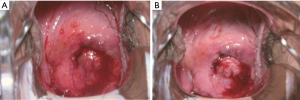
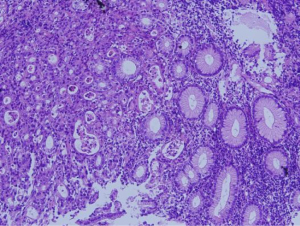
On December 23, 2019, she returned to hospital for review as she was still experiencing vaginal bleeding whilst on medication, although the amount was less than before. Gynecological examination revealed an enlarged, barrel-shaped cervix barrel-shaped with a diameter of 5 cm, with obvious bleeding on the surface and a brittle texture involving the posterior fornix. The right main ligament shortened to the pelvic side wall, and the left main ligament shortened to involve the pelvic side wall. Vaginal B-ultrasound showed that the anterior and posterior diameter of the cervix was 3.4 cm, the size of the cystic solid space was 5.5×4.3×4.8 cm on the right ovary, with an irregular shape and relatively clear cystic fluid (Figure 1). There were no abnormalities in cervical liquid-based cytology or HPV testing. The level of CA-199 was 1,377 U/mL and all other tumor markers were normal. Colposcopy showed that the surface of the cervix had obvious bleeding, and was brittle and enlarged with a diameter of 5+ cm. A cauliflower-like lesion of 1+ cm was seen in the cervix. Following an acetic acid white test, thick white epithelium and abnormal blood vessels were observed and multiple-points biopsy was performed (Figure 2). The enhanced computed tomography (CT) scan of the pelvic and abdominal cavity showed a cystic solid space in each appendix area; the size of the right side was about 4.2×6.8×10.3 cm, and the size of the left side was about 4.5×3.3×4.4 cm. The solid components could be enhanced, and the two sides formed an ovarian pedicle sign. The size of the cervix increased to 4.1×3.8×4.2 cm, reaching the junction of the neck and body. The bilateral sacral ligaments were obviously thickened and strengthened. We considered two diagnoses: (I) cervical malignant tumor; (II) cervical metastatic cancer. The cervical biopsy results showed a poorly differentiated mucinous adenocarcinoma, with signet ring cell carcinoma differentiation in some areas, and a tumor thrombus in the vessel; ICH: tumor cells: cytokeratin (CK)7++, CK20+, CDX-2+, CEA+++, SATB2-, ER-, PR-, P53-, Villin+++, Muc-2++, Muc-5 focus+, CA199++, P16++, ki-67 positive rate 70–90% (Figure 3). The results of immunohistochemistry analysis suggested metastatic cancer from a digestive system tumor. Gastrointestinal endoscopy showed rectal mucosal swelling with lumen stenosis. The pathological results of a gastric mucosa multi-point biopsy showed poorly-differentiated mucinous adenocarcinoma and signet ring cell carcinoma were found. A rectal mucosal biopsy specimen showed mild chronic inflammation but no tumors (Figure 4).

On January 14, 2020, the patient was transferred to the Department of Oncology, West China Hospital, Sichuan University, where she was diagnosed with poorly‑differentiated adenocarcinoma of the gastric antrum (including some signet ring cell carcinoma) with bilateral adnexa and cervical metastasis. After evaluation by the multi-disciplinary team (MDT), a preliminary treatment plan was formulated: after neoadjuvant chemotherapy, the potential for surgery was evaluated. Starting from January 16, 2020, the patient began treatment on a FLOT regimen (Oxaliplatin 100 mg ivgtt d1; Docetaxel 60 mg ivgtt d1; Leucovorin 0.6 g ivgtt d1; Fluorouracil 1,750 mg civ 46h d1~2, Q2w) for 4 cycles. On April 11th, considering the progression of the disease, she switched to a second-line FOLFIRI regimen (Irinotecan 280 mg d1, Levoleucovorin 235 mg d1, 5-Fu 650 mg ivgtt d1, 5-Fu 1,875 mg civ 24h d1~2, Q3w) for 2 courses. On May 1, 2020, the patient developed hemorrhagic shock due to rupture of the metastatic lesion in the ovary. After anti-shock therapy, interventional hemostasis and other treatments, the patient’s condition did not improve. After discussion, the MDT decided to perform an exploratory laparotomy and hemostasis was performed by bilateral salpingo oophorectomy in the emergency department on May 6, 2020. The patient recovered well after surgery. Upon postoperative examination, there was widespread necrosis and adenocarcinoma metastasis in the right ovary and fallopian tube. The patient is currently in a stable condition and is undergoing chemotherapy.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Cervical metastases are rare, and metastases from organs outside the pelvic cavity are even more rare. Most are case reports or retrospective analyses of small patient populations. The incidence of cervical metastases is only 0.3%, and the average age at diagnosis of metastatic cancer is 44 years (23–75 years) (1-3). According to literature reports (4), among metastatic cervical cancers, ovarian cancer metastasized to the cervix accounts for 36.4% of cases, colorectal cancer accounts for 30.3%, gastric cancer accounts for 15.2%, breast cancer accounts for 12.1%, renal cell carcinoma and transitional cell carcinoma of renal pelvis account for 3.0% each. Gastric cancer metastasis to the cervix is mostly reported as gastric cancer recurrence and metastasis to the cervix, and cervical cancer as the primary manifestation is very rare. There have been fewer than 10 cases reported in the literature. The youngest patient reported to date was 29 years old (2,5). We present a case of cervical metastases from gastric cancer in a 22-year-old patient, which is the youngest reported so far. It has been reported that 76.9% of patients with cervical metastasis from gastric cancer are younger than 50 years old, suggesting that the relatively high blood flow to the cervix of relatively young patients may be an important cause of cervical metastasis (3).
The clinical manifestations of cervical metastatic cancer are similar to those of primary cervical cancer, most of which are irregular vaginal bleeding, which is easy to be misdiagnosed when there is no history of a primary tumor. Most patients with cervical metastatic cancer have cervix enlargement and hardening with some nodular lesions, and 50% of patients have no observable abnormalities in the cervix upon pelvic examination (2,6). Imachi et al. (2) analyzed the clinicopathological data of 16 patients with cervical metastases from gastric cancer and found that 43.7% of patients had normal cervical cytology, whilst 57.1% had normal colposcopy results, and about half of patients with cervical metastases could not pass routine cervical cancer screening. In this case, the patient was only 22 years old and had no history of gastrointestinal disease. We found that her cytology and HPV test results were normal, and the cervix was only erosive and bloody during the previous gynecological examination, which made the diagnosis difficult. This case suggests that routine cervical cancer screening has a high false-negative rate in the diagnosis of metastatic cervical cancer, and this must be addressed to reduce the occurrence of missed diagnosis and incorrect diagnosis.
Malignant tumors from organs outside the pelvis that metastasize to the cervix have obvious histological characteristics of the primary tumors, which can provide a basis for clinicians to identify the primary tumor and make a clear diagnosis. Such cases mainly involve the deep interstitium of the cervix, without the transformation process of precancerous lesions, and the squamous-columnar junction is often not involved (7). The histological tumor subtypes from patients with gastric cancer and cervical metastasis are mostly signet ring cell carcinoma and poorly-differentiated adenocarcinoma, accounting for 64.7% and 20.6% of cases, respectively (3). The results of immunohistochemistry showed that CK7, CK20, CDX-2, and carcinoembryonic antigen were positive, which indicated the possibility of gastrointestinal metastasis. At present, there are no reports of HPV detection in patients with metastatic cervical cancer. HPV was not detected in this patient; however, the immunohistochemical results showed that p16 (one of the markers of HPV infection) was positive, which was a conflicting result. However, evidence suggests that 75% of patients with gastric cancer are positive for p16 (8), so it is necessary to differentiate these cases from HPV-negative primary cervical cancer.
According to the literature, 20–40% of metastatic cervical cancer cases are misdiagnosed as primary cervical cancer (1,9). It is very important to ask carefully about the medical history and family history, and the following must be observed: (I) exclude primary cervical cancer; (II) find the location of the primary cancer; (III) signet-ring cell-like non-Hodgkin’s lymphoma, signet-ring cell-like melanoma, cervical non-neoplastic signet-ring cell-like changes and other diseases, if necessary, CK, leukocyte common antigen HMB45, and S-100 should be analyzed (10,11).
The prognosis of patients with metastatic cervical cancer is poor. The main factors affecting prognosis are the location of the primary tumor and the degree of malignancy, pathological type and treatment methods. It has been shown that the average overall survival time of patients with primary ovarian cancer, colorectal cancer, gastric cancer, breast cancer, and renal cell carcinoma cervical metastasis is 8, 8.3, 1.8, 6.4, and 10 months, respectively (4). The average overall survival time for signet ring cell carcinoma, mucinous adenocarcinoma, and high/medium/poorly-differentiated adenocarcinoma is 10, 13, and 18.1 months, respectively. Signet ring cell carcinoma with gastric metastasis to the cervix has the worst prognosis, with an average overall survival time of 5.5 months (5,12).
There is no standard for the treatment of metastatic cervical cancer. Studies have shown that overall survival with comprehensive treatment is longer than for radiotherapy or surgery alone (17.7 vs. 10.7 or 13.2 months, respectively). Mean overall survival following radical surgery combined with radiotherapy and chemotherapy was significantly longer than cytoreductive surgery (22.3 vs. 7.8 months, respectively). Therefore, we would advise that patients who are able to undergo surgery should choose a comprehensive treatment plan including surgery to achieve radical cure or maximum tumor reduction, followed by postoperative adjuvant radiotherapy and chemotherapy to control subclinical foci and possible metastases and postoperative residual lesions (12). Suárez-Peñaranda et al. (5) found that no patients with metastatic signet ring cell carcinoma of the cervix survived for more than 11 months, and most patients died within 6 months. The authors noted that compared with surgery alone, combined surgery, radiotherapy and chemotherapy can prolong tumor-free survival. Most patients with cervical metastases also have multiple pelvic organ involvement. Metastases in other distant sites were found before, during and after treatment in our patient. Therefore, effective diagnosis and treatment is paramount for metastatic cervical cancer.
Conclusions
Metastatic cervical cancer is rare. Young type gastric signet ring cell carcinoma with cervical metastasis as the only first symptom is extremely rare. It is easy to be ignored and delayed in diagnosis and treatment. The prognosis is poor. There is no effective and unified treatment plan. Clinical diagnosis and treatment should be taken seriously.
Acknowledgments
Funding: The Key Project of Sichuan Provincial Department of Science and Technology: “Study on the key factors affecting the diagnosis and treatment of major diseases in obstetrics and gynecology (19ZDYF)” (Approvalled Medical Ethics Committee of West China Second University Hospital, Sichuan University. Ethical Lot Number: 20200076).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-32/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-32/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-32/coif). All authors report that they receive consulting fees from funding: The Key Project of Sichuan Provincial Department of Science and Technology: “Study on the key factors affecting the diagnosis and treatment of major diseases in obstetrics and gynecology (19ZDYF)” (Approvalled Medical Ethics Committee of West China Second University Hospital, Sichuan University. Ethical Lot Number: 20200076). RY serves as an unpaid editorial board member of Gynecology and Pelvic Medicine from June 2020 to May 2022. The authors have no other conflicts of interests to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mazur MT, Hsueh S, Gersell DJ. Metastases to the female genital tract. Analysis of 325 cases. Cancer 1984;53:1978-84. [Crossref] [PubMed]
- Imachi M, Tsukamoto N, Amagase H, et al. Metastatic adenocarcinoma to the uterine cervix from gastric cancer. A clinicopathologic analysis of 16 cases. Cancer 1993;71:3472-7. [Crossref] [PubMed]
- Yamamoto T, Mori T, Matsushima H, et al. Late, isolated metastasis from poorly differentiated gastric cancer to the uterine cervix. Gynecol Oncol Case Rep 2014;8:17-20. [Crossref] [PubMed]
- Lemoine NR, Hall PA. Epithelial tumors metastatic to the uterine cervix. A study of 33 cases and review of the literature. Cancer 1986;57:2002-5. [Crossref] [PubMed]
- Suárez-Peñaranda JM, Abdulkader I, Barón-Duarte FJ, et al. Signet-ring cell carcinoma presenting in the uterine cervix: report of a primary and 2 metastatic cases. Int J Gynecol Pathol 2007;26:254-8. [Crossref] [PubMed]
- Yang Z. A report of 11 cases of cervical metastasis from gastric cancer. Cancer Research on Prevention and Treatment 1996;6:361-2.
- Hartsough EM, Erickson BK, Chauhan A, et al. Isolated metastatic pancreatic adenocarcinoma to the uterine cervix: A case report. Gynecol Oncol Rep 2019;29:61-3. [Crossref] [PubMed]
- Schneider BG, Gulley ML, Eagan P, et al. Loss of p16/CDKN2A tumor suppressor protein in gastric adenocarcinoma is associated with Epstein-Barr virus and anatomic location in the body of the stomach. Hum Pathol 2000;31:45-50. [Crossref] [PubMed]
- Pérez-Montiel D, Serrano-Olvera A, Salazar LC, et al. Adenocarcinoma metastatic to the uterine cervix: a case series. J Obstet Gynaecol Res 2012;38:541-9. [Crossref] [PubMed]
- Yin Z, Xia J, Wang Y, et al. Expression and significance of MITF, S-100 protein and HMB45 in melanoma and pigmented nevus. Chinese Journal of Laboratory Diagnosis 2011;15:2039-40.
- Ragazzi M, Carbonara C, Rosai J. Nonneoplastic signet-ring cells in the gallbladder and uterine cervix. A potential source of overdiagnosis. Hum Pathol 2009;40:326-31. [Crossref] [PubMed]
- Yin Z, Yu H. Clinical analysis of 22 cases of cervical metastasis from gastric cancer and colorectal cancer. Chinese Journal of Cancer 2009;19:210-3.
Cite this article as: Zhang M, Li K, Yin R. Gastric cancer in a 22-year-old woman with metastasis to the cervix: a case report and literature review. Gynecol Pelvic Med 2022;5:21.


