
Rare multiple teratomas of the omentum and giant fused teratomas of the bilateral ovaries: a case report and review of the literature
Introduction
Mature teratoma, also known as dermoid cysts or benign cystic teratoma, is one of the most common benign ovarian tumors (1). The incidence of teratoma in females has been shown to be much higher than that in males, due to the location of the ovary (2). A mature teratoma is usually benign with the definitive treatment being entirely based on surgery; in contrast, an immature teratoma requires sequential chemotherapy and/or radiotherapy (3,4). Teratomas have been demonstrated to have a predisposition to grow on or to invade and disrupt the ovarian parenchyma and/or adnexa as a consequence of its germ cell–derived characteristics. However, teratomas of the omentum are fairly rare. The first case of omental teratoma was described by Lebert in 1734 (5), and fewer than 46 cases have been described thus far, with Mumey et al. reporting 15 cases and Kearney et al. reporting 12 cases (6,7). We present the following article in accordance with the CARE reporting checklist (available at https://gpm.amegroups.org/article/view/10.21037/gpm-21-35/rc).
Case presentation
A 47-year-old woman, gravida 3 and para 1, was admitted to our hospital with intermittent distending pain and discomfort, which became aggravated during duration of menstruation and had lasted for over half a year. She had no history of trauma, surgery, or gynecologic problems, except for 1 induced abortion 23 years ago. On admission, general physical examination showed no abnormality. However, during pelvic examination, cervical hypertrophy and several Nabothian cysts were revealed. Her uterus was found anteverted, anteflexed, and of normal size while the mobility was relatively poor. A nontender, fluctuant, and movable cystic mass with unclear borderlines was palpable on the bilateral adnexa. Transvaginal ultrasound scan showed an irregular cystic space–occupying lesion, measuring 4.2×3.8×3.7 cm, which encompassed the right ovary. Meanwhile, two cystic masses were detected in left adnexa area with one measuring 3.6×2.8×2.5 cm showing flocculent echo and the other measuring 3.4×3.4×2.4 cm displaying clear cyst fluid (Figure 1). Her carbohydrate antigen (CA) 125 level was 99.9 U/mL (normal, <35 U/mL), her CA 19-9 was 80.4 U/mL (normal, <30.9 U/mL), and her α-fetoprotein (AFP) level was 12.5 ng/ml, which was slightly higher than normal level (8.1 ng/mL). The other preoperative laboratory tests, including the biochemical tests, complete blood count, urinalysis, and blood coagulation profile were normal.
Laparoscopic exploration with laparoscopic ovarian cystectomy was planned. However, during the laparoscopic exploration, the atrophic uterine was found adhering to the bilateral ovaries broadly and tightly. On the left ovary, several cysts measuring up to 4–10 cm had fused to become a giant mass around 20×18×14 cm, while a similar mass measuring 10×8×5 cm was observed on the right side; other multiple masses with diameters over 1–5 cm were found attached to the greater omentum, which was in turn adhering broadly to the bowel and pelvic area. After communicating with her family members, the surgeon converted laparoscopy to laparotomy. The intraoperative frozen section showed mature cystic teratoma. The final surgery that was performed was laparotomy combined with hysterectomy, bilateral salpingo-oophenrectomy, omentectomy, appendicectomy. and enterolysis. Till now, the patient has recovered well during the follow-up of 8 years.
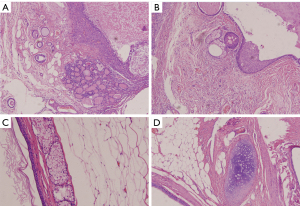
Macroscopically, the excised specimen was described as an irregular mass of tissue encircling the ovaries and being firmly attached to the omentum. A cross-section of the teratoma revealed giant cysts harboring hair, teeth and pultaceous, adipose material (Figure 2). Microscopically, the pathologic specimen was confirmed as typical cystic mature teratomas with some ovarian stroma, which consisted of thyroid follicular tissue and skin appendage with squamous epithelia. Pathologic examination of the omental specimen showed keratinized tissue, mature adipose tissue, sebaceous glands, and cartilage tissue, which were all common content of mature teratoma (Figure 3).

All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
iMDT discussion
Discussion among physicians from the West China Second University Hospital of Sichuan University
Teratoma of the omentum is rare, with only few reports of this condition (8,9) however, the presence of lesions on the bilateral ovaries and the omentum is even rarer, with only 1 previous report on this (7). The reason why teratoma develops on the omentum is not well understood. Three main theories have been proposed to explain their location. (I) Primary teratomas of the omentum may originate from displaced germ cells. (II) Teratomas may develop in a supernumerary ovary of the omentum. (III) Teratomas may result from auto-amputation of an ovarian dermoid cyst with secondary implantation into the greater omentum (10,11).
We performed a PubMed search using the key words “omentum”, “teratoma” or “ovarian teratoma”, “dermoid cyst”, and a search of the collected literature was performed to identify previously reported cases from January 1928 to December 2019. Cases were limited to the English literature. Titles and abstracts were reviewed independently by two authors (TL and TC). Disagreements were resolved by discussions between the two reviewers (WZ and JH). Only case reports or cases series of omentum teratomas were included. The cases required to be diagnosed as mature or immature teratoma of the greater omentum or lesser omentum teratoma bases on histopathological evidence from surgery. Finally, 44 articles and meeting abstracts with a total of 46 cases were included. A summary of the 47 cases (including our own cases) is shown in Table 1. The first case of omental teratoma was described by Lebert (5) in 1734. Forty-four international reports (46 cases) on the omental teratoma have been published since Mumey’s report in 1928. Primary omental teratoma occurs more commonly in females than in males, with the average of the males being much younger than of the females, and malignant transformation (MT) is rare. As shown in the Table 1, there are 43 female cases and the remaining four are male cases. The reported average age of the female patients was 42.9 years (range, 12–83 years), while that of male patients was 8.7 years (range, 8 months to 27 years). The reported tumor size varied widely, ranging from 2 cm in diameter to the maximum size of 85×75×5 cm. Three male cases were reported in lesser omentum (19,24,30). Three cases involved histologically immature teratomas, and the patients required postoperative chemotherapy and radiotherapy. One case was defined as MT of a mature cystic teratoma of the omentum (23). Thirteen cases were coexistent with benign teratoma of ovary; two cases were coexistent with mucinous cystadenoma, five cases were coexistent with agenesis or atrophy of the gonads, only one case was coexistent with mature cystic teratoma of the right ovary, pouch of Douglas and the abdominal wall. Our case was only coexistent with benign teratoma of bilateral ovaries. In most cases the chief complaint was abdominal pain. However, the symptoms were not uniform; in some cases, it was very acute and in others the patients complained of occasional pain.
Table 1
| Authors, years | Age (years) | Sex | Tumor size | Microscopic findings | Associated pathologic findings |
|---|---|---|---|---|---|
| Mumey N, 1928 (6) | 35 | F | 5 cm in diameter | Dermoid cyst | – |
| Love RJM, 1930 (12) | 53 | F | Cricket-ball size | Dermoid cyst | – |
| Lazarus JA, 1931 (5) | 48 | F | 85×75×55 cm | Dermoid cyst | Left ovarian dermoid cyst |
| Judd ES, 1933 (13) | 52 | F | 5 cm in diameter | Dermoid cyst | Right ovarian dermoid cyst |
| Warfield JO, 1956 (14) | 69 | F | 8×5×4 cm | Dermoid cyst | – |
| Hogan ML, 1967 (15) | 21 | F | 11×7×4.5 cm | Benign cystic teratoma supernumerary omental ovary with benign cystic teratoma (dermoid cyst) | – |
| Printz JL, 1973 (16) | 23 | F | 5×4 cm | Benign cystic teratoma | Benign cystic teratoma of left ovary |
| Ekbladh LE, 1973 (17) | 41 | F | 6×6 cm | Dermoid cyst | Left ovary hypotrophy |
| Bell DA, 1980 (18) | 53 | F | 32×6×15 cm | Benign cystic teratoma | Benign cystic teratoma of right adnexa |
| Kearney MS, 1983 (7) | 70 | F | 7×5×3.5 cm | Benign teratoma | Left ovarian cyst |
| Ordonez NG, 1983 (19) | 22 | F | 2 cm in diameter | Immature teratoma | – |
| Compton AA, 1985 (20) | 39 | F | 8×7 cm | Mature cystic teratoma | Mature cystic teratoma of left ovary |
| Leno C, 1987 (21) | 66 | F | 8×6×6 cm | Dermoid cyst | Atrophy of left ovary |
| Ralls PW, 1987 (22) | 45 | F | 5×5 cm | Benign cystic teratoma | Cystic teratoma of left ovary |
| Spurney RF, 1987 (23) | 12 | F | 30×15×9 cm | Immature teratoma | – |
| Mercer LJ, 1987 (24) | 34 | F | 18.5×12×8.5 cm | Benign cystic teratoma | – |
| Deppe G, 1988 (25) | 31 | F | 11×8×7 cm | Mature cystic teratoma | – |
| Drut R, 1990 (26) | 2 | M | 5×5×4 cm | Mature solid teratoma | Agenesis of left testis |
| Smith R, 1990 (10) | 68 | F | 6×5 cm | Mature teratoma | Mucinous cystadenoma of left ovary |
| Whang SH, 1990 (27) | 34 | F | NA | Mature teratoma | – |
| Besser MJ, 1992 (28) | 47 | F | 7×5×4 cm | Cystic teratoma | – |
| Kriplani A, 1995 (29) | 36 | F | 7×6 cm | Dermoid cyst | Agenesis of bilateral oviduct and ovary |
| Furuhashi M, 1997 (30) | 28 | F | 7.5×6.5 cm | Cystic teratoma | – |
| Mazumdar A, 1997 (8) | 50 | F | 12×10 cm, 4×2 cm | Dermoid cyst (multiple) | – |
| Moon WJ, 1997 (31) | 57 | F | 8×8×7 cm | Cystic teratoma | Cystic teratoma of left ovary |
| Moon WJ, 1997 (31) | 53 | F | 4×4×5 cm | Cystic teratoma | Cystic teratoma of left ovary |
| Ushakov FB, 1998(1) | 36 | F | 10×9 cm | Benign cystic teratoma | Benign cystic teratoma of left ovary |
| Ushakov FB, 1998 (1) | 27 | F | 4×5 cm | Benign cystic teratoma | – |
| Patankar T, 1999 (32) | 5 | M | NA | Benign cystic teratoma | – |
| Ollapallil J, 2002 (33) | 46 | F | 11×4×3 cm | Benign cystic teratoma | – |
| Pfitzmann R, 2004 (34) | 36 | F | 9 cm in diameter | Dermoid cyst | – |
| Yoshida A, 2005 (35) | 36 | F | 5×4×4 cm | Mature cystic teratoma | Atrophy of left ovary |
| Kubosawa H, 2006 (36) | 62 | F | 7×6×4 cm, 2 cm in diameter | Adenocarcinomas, benign cystic teratoma (multiple) | – |
| Baviskar BP, 2006 (37) | 8 mo | M | 14 cm in diameter | Benign teratoam | – |
| Chen SS, 2008 (38) | 35 | F | 15 cm in diameter | Mature tertoma | – |
| Sinha R, 2009 (39) | 23 | F | NA | Mature cystic teratoma | Mature cystic teratoma of the right ovary, pouch of Douglas and the abdominal wall |
| Ali AA, 2009 (40) | 55 | F | 3×3 cm | Mature cystic teratoma | - |
| Wani BN, 2011 (41) | 9 | F | 17×13×10 cm | Mature cystic teratoma | - |
| Richardson R, 2011 (42) | 27 | F | 12x7.3x5.5 cm | Immature tertoma | - |
| Hardesty BM, 2012 (43) | 27 | M | 8.5×7.9×7.0 cm | Mature cystic teratoma | - |
| Sforza M, 2012 (44) | 82 | F | 10 cm in diameter | Mature cystic teratoma | - |
| Schols RM, 2013 (45) | 83 | F | 9.5×6×5.5 cm | Benign dermoid cyst | - |
| Hegde P, 2014 (46) | 26 | F | 7×7 cm | Benign cystic teratoma | Benign cystic teratom of right ovary |
| Kim TH, 2014 (47) | 38 | F | 2 cm in diameter | Benign teratoma | - |
| Rampinelli F, 2017 (48) | 54 | F | 6 cm in diameter | Benign cystic teratoma | - |
| Huang CC, 2019 (49) | 34 | F | 5 cm in diameter | Benign cystic teratoma | Mucinous cystadenoma of right ovary |
| Present case | 47 | F | 1~5 cm in diameter | Mature cystic teratoma | Mature cystic teratoma of bilateral ovaries |
As for diagnosis for this condition, transvaginal ultrasonography is optimal, with both sensibility and specificity being shown to be sufficient (50,51). However, in our case, preoperative detection and diagnosis were dependent on ultrasonography, yet a severe misdiagnosis occurred: these masses were either located too deep in the pelvic area or in the umbilicus adjacent to the epigastric area, and only a tiny fraction of the bilateral ovarian cysts was detectable. The initial examination thus completely missed the omental teratomas, suggesting that the transvaginal ultrasonography may not be foolproof in the diagnosis of this condition. Thus, we recommend more comprehensive radiological examinations, such as abdominal and pelvic computed tomography (CT) or magnetic resonance imaging (MRI) (52), before operation to confirm the diagnosis and optimize the surgical plan.
Our patient had 2 giant ovarian teratomas and multiple ones attached to the omentum, which could not be removed completely under the laparoscopic view, requiring us to switch to laparotomy. Considering the age and basic condition of the patient, the surgical incision was made as small as possible, and we chose to remove the cysts after draining out the cystic fluid to reduce the length of incision, as indicated by Baris et al. (53). Currently, no standardized operation approach has been recommended by authoritative guidelines for this condition. Vertical incision will be more appropriate in cases with suspected malignancy in order to be able to enlarge the incision, especially in the giant mass. Gynecologist could either extend the incision to preserve the integrity (54) of the cyst or decompress the cyst prior to removal (55,56). In our case, because the malignant of giant masses cannot be ruled out, we performed intraoperative frozen sections evaluation. Intraoperative frozen section analysis is of utmost importance for planning a proper surgical management (57). Frozen section analysis is a very useful intraoperative diagnostic tool, with a turnaround time of 15 to 20 minutes, that especially aids in the categorization of tumors as benign, borderline and malignant, thus guiding in determining the extent of surgery, the overall accuracy of frozen section in diagnosing malignancy was 99.34% (58). The final diagnosis was determined after laparotomy and subsequent pathological examination. The benign teratoma was treated by operation, and prognosis is good. In our case, no recurrence has been observed as of 8 years following the operation.
What are the operational difficulties and precautions involved in the laparoscopic surgery for multiple teratomas?
Expert opinion 1: Qmer Lutfi Tapisiz
- Residual tumor may remain in multiple teratoma operations. We should make detailed anatomical mapping for mutiple teratomas in preoperative period by ultrasonography and/or magnetic resonance imaging. Then, we can/should remove all teratomas with its guidance.
- As teratomas increase in size, laparoscopic removal may be difficult. Also, If there is a risk of preoperative immature teratoma, it is important that the tumor should not rupture as much as possible to prevent upstaging. This can be difficult in laparoscopic approach.
- Large teratomas in the omentum can be difficult to remove laparoscopically.
- Intraoperatively, frozen section evaluation is very important for adnexal masses. This evaluation was not performed in our case. This limitation of our case report should be discussed and its importance should be stated in the text.
Expert opinion 2: Andrea Giannini, Ricardo Bassll Lasmar, Bernardo Portugal Lasmar
In a similar scenario it is essential to perform an accurate exploration of the peritoneal cavity and the surface of the parenchymal organs of the upper abdomen, and this task could be more difficult in laparoscopy than in laparotomy, especially if extra-pelvic masses are very bulky. It may be necessary to place the trocars in different points from the usual ones or to resort to additional laparoscopic accesses. If the number of peritoneal implants is not excessive, we could first of all remove them with an endobag and determine their nature whit a frozen section (59). It is reasonable to believe that the laparoscopic approach is associated with a higher risk of iatrogenic rupture of these multiple solid-cystic masses than that evidenced for adnexal teratomas. If this occurs it may be more difficult to perform a thorough washing of the entire peritoneal surface to prevent chemical peritonitis and chronic granulomatous peritonitis (60). Thus, the challenge of the surgery is the preservation of the ovarian parenchyma, using as little cauterization as possible, and the removal of the piece always in endobag, as a complication of the surgery is chemical peritonitis due to sebaceous cyst fluid leakage.
What is the potential impact of preserving fertility function in multiple teratomas if the patient wants to preserve fertility?
Expert 1: Andrea Giannini
As in single teratoma, also in multiple teratomas the ovarian reserve depends on the volume of residual healthy ovarian parenchyma. When ovarian cystectomy is feasible, a careful tissue handling and limited use of electrosurgery are mandatory for fertility sparing (6). Sometimes it is not possible to perform cystectomy without damaging little residual healthy tissue. When this happens in both annexes, for the purpose of preserving fertility, a more effective strategy could consist only in removal of the peritoneal implants and in the resolution of any adhesions between fallopian tubes and other structures that could cause the malfunction of the tubes. This is possible if the size of dermoid cysts is not excessive, otherwise the risk of spontaneous complications such rupture and torsion is very high (61). In these cases, sclerotherapy, already used for endometriomas, could represents a therapeutic option in the future (62). Follow-up based on serial ultrasound evaluation should be performed to check the size and rule out signs indicative of malignant evolution.
Self-amputation and reimplantation appear to be the main mechanisms underlying the formation of multiple teratomas. This often leads to atrophy of the residual ovarian parenchyma and the simultaneous creation of a dead-end fallopian tube (1). For this reason and for the frequent distortion and compression of the fallopian tubes due to the voluminous pelvic dermoid cysts methylene blue test for assessment of tubal patency could better clarify the reproductive potential of the patient.
Expert 2: Qmer Lutfi Tapisiz, Ricardo Bassll Lasmar, Bernardo Portugal Lasmar
If appropriate anatomical mapping is performed preoperatively in multiple teratomas by USG and/or CT, MRI; all teratomas can be gently removed by cystectomy with preserving ovaries (fertility). Use as little coagulation as possible, make a blunt dissection of the capsule, avoid the rupture of the cyst at all costs. Remove the cyst with an endobag.
However, intraoperative frozen section should be performed to exclude the malignencies and all teratomas should be removed under the preoperative imaging guidance. However, no matter how much the ovaries are preserved, the patient and their relatives should be informed before the operation that the ovaries will be affected.
What is the optimal treatment for multiple teratomas?
Expert 1: Andrea Giannini
The best strategy for the patient could be a cautious approach involving peritoneal lavage with cytological examination and subsequent removal in endobag of one or more peritoneal implants. The accurate histopathological analysis of the samples, the dosage of tumor markers and a preoperative imaging extended to the entire abdomen with CT scan and possibly also MRI and PET, will help to better define the exceptional benign nature of this disease and therefore to plan a conservative and more conscious surgical effort (59). Alternatively, we could perform a frozen section of peritoneal nodules and, once the benign nature is known, proceed with only the removal of all other dermoid cysts. However, in this situation, the extemporaneous histopathological analysis could have a very poor diagnostic accuracy given the frequent large sample size and the bizarre related clinical information.
Expert 2: Qmer Lutfi Tapisiz, Ricardo Bassll Lasmar, Bernardo Portugal Lasmar
If the patients want to preserve fertility, all teratomas can be gently removed by cystectomy with preserving ovaries. In perimenopausal patients, hysterectomy with bilateral oophorectomy is more suitable for definitive treatment. Surgery. Preferably the laparoscopic or robotic route. The amplification of vision allows for a more delicate and conservative surgery, with greater chances of removal of the whole cyst and preservation of the ovarian parenchyma.
Does the autoamputation of mature ovarian teratoma increase the risk of MT?
Expert 1: Ricardo Bassll Lasmar, Bernardo Portugal Lasmar
Ovarian teratoma may underwent torsion, autoamputation, and reimplantation. A frequent place of reimplantation is the omentum, became a parasitic teratoma. It may keep the risk of MT if not removed, but the risk does not seem to be increased. MT is very rare, occurring in only 0.5% to 2% of mature teratoma cases. The most frequent malignancy arising in mature teratomas is squamous cell carcinoma.
Expert 2: Qmer Lutfi Tapisiz
MT is very rare, occuring in only 0.3–4.8% of mature teratoma cases. MT usually occurs in postmenopausal women and may be associated with higher tumor diameter *. I could not find any information in the English literature about autoamputation increase the risk of MT. However, a proliferative microenvironment is formed for the tissue to hold in the omentum after autoamputation. Although there is no evidence, it can be speculated that this proliferative microenvironment may lead to increase the risk of MT (63).
Expert 3: Andrea Giannini
Self-amputation appears to be the main mechanism underlying the formation of multiple teratoma. It probably occurs as a result of a torsion of the adnexal dermoid cyst with consequent ischemia and hypoxia of a portion of the mass. This event can be acute, subacute or chronic. It is very likely that only a subacute or chronic hypoxic stimulus can avoid necrosis and trigger an increased expression of genes coding for molecular factors of neo-angiogenesis. In fact, neo-angiogenesis is certainly a determining process for the reimplantation of parasitic cysts. The revascularization of the tumor portions not undergoing necrosis but still subjected to a marked hypoxic stimulus could cause the formation of a large amount of oxygen free radicals which could increase the genomic instability of the tumor and therefore increase the probability of malignant evolution. In addition, it is likely that torsion is associated with a chronic inflammatory state which could favor the development of immunotolerance towards tumor cells and progression of cancer (64).
How can teratoma of the omentum be diagnosed?
Expert 1: Ricardo Bassll Lasmar, Bernardo Portugal Lasmar
The best exam to diagnose it is MRI, the sebaceous component of dermoid cysts has very high signal intensity on T1-weighted images, similar to retroperitoneal fat. The signal intensity of the sebaceous component on T2-weighted images is variable, usually approximating that of fat.
Expert 2: Qmer Lutfi Tapisiz
It should be performed abdominal USG in addition to TVUSG in suspected adnexal masses. If a suspicious intra-abdominal lesion is detected in the abdominal USg (like omental mass, etc.), CT or MRI must be performed for differential diagnosis of the mass and preop operation planning.
Expect 3: Andrea Giannini
Regardless of their location teratomas have often characteristic sonographic findings. However, an exhaustive study of an extra-pelvic expansive mass, like a teratoma of omentum, cannot be performed with ultrasound evaluation alone, even when it shows sonographic signs typical of adnexal teratoma. More advanced imaging techniques, first of all CT scan, MRI and possibly also the PET, must be used to better define the qualitative tissue composition, the relationship between the mass and the nearby structures, the metabolic activity, and the possible presence of other lesions in the rest of the abdomen. Teratomas, especially those with omental localization, could confuse with other fatty tumor masses like lipoleiomyomas (65). In any way, despite the most modern imaging techniques have shown a high diagnostic accuracy in detection of these tumor masses, currently a definitive diagnosis of omental teratoma is obtained only with histological analysis.
Conclusions
We reported a rare case of multiple teratomas of the omentum and giant, fused teratomas of the bilateral ovaries. Histopathological studies confirmed the teratomas, and surgery completely resolved the original symptoms. The reasons for teratomas forming on the omentum are not well understood. There is no standard diagnostic criteria or operative options for omental teratomas, and thus misdiagnosis may occur and preoperative planning may be suboptimal. Ultrasound, CT, MRI and possibly also the PET may aid in the diagnosis. A definitive diagnosis is possible following histopathological examination, which must differentiate between mature and immature teratoma. Although, MT of the omentum teratoma has been described, the risk is very rare. Surgical excision of omentum teratoma is the treatment of choice, and most surgeons perform laparoscopy with tumor dissection. The surgical technique remains particularly important especially in young women, in whom the most conservative approach is crucial, to preserving fertility and minimizing surgical morbidity. The management depends upon the maturity of the teratoma. For mature teratoma, complete excision is curative and no further treatment is required. Immature teratomas are potentially malignant, so the patient may require chemotherapy and radiotherapy.
Acknowledgments
Funding: This study was supported by the National Natural Science Foundation of China, Beijing, China (no. 81101991) and the Interrelation-Oriented Multidisciplinary Training Program, Sichuan University (no. SCUKG071). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the article.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “iMDT Corner”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.org/article/view/10.21037/gpm-21-35/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.org/article/view/10.21037/gpm-21-35/coif). The series “iMDT Corner” was commissioned by the editorial office without any funding or sponsorship. YS serves as an unpaid editorial board member of Gynecology and Pelvic Medicine from May 2021 to Apr 2023. OLT serves as an unpaid editorial board member of Gynecology and Pelvic Medicine from Dec. 2020 to Nov. 2022. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ushakov FB, Meirow D, Prus D, et al. Parasitic ovarian dermoid tumor of the omentum-A review of the literature and report of two new cases. Eur J Obstet Gynecol Reprod Biol 1998;81:77-82. [Crossref] [PubMed]
- Mann JR, Gray ES, Thornton C, et al. Mature and immature extracranial teratomas in children: the UK Children's Cancer Study Group Experience. J Clin Oncol 2008;26:3590-7. [Crossref] [PubMed]
- Alborzi S, Foroughinia L, Kumar PV, et al. A comparison of histopathologic findings of ovarian tissue inadvertently excised with endometrioma and other kinds of benign ovarian cyst in patients undergoing laparoscopy versus laparotomy. Fertil Steril 2009;92:2004-7. [Crossref] [PubMed]
- Kurata A, Hirano K, Nagane M, et al. Immature teratoma of the ovary with distant metastases: favorable prognosis and insights into chemotherapeutic retroconversion. Int J Gynecol Pathol 2010;29:438-44. [Crossref] [PubMed]
- Synchronous dermoid cyst of great omentum and ovary. Available online: https://saspublishers.com/media/articles/SASJS-42-38-42-c.pdf
- Mumey N. Dermoid cyst of greater omentum. Am J Surg 1928;5:56-60. [Crossref]
- Kearney MS. Synchronous benign teratomas of the greater omentum and ovary. Case report. Br J Obstet Gynaecol 1983;90:676-9. [Crossref] [PubMed]
- Mazumdar A, Vaiphei K, Verma GR. Multiple dermoid cysts of omentum. J Postgrad Med 1997;43:41-2. [PubMed]
- Patel F, Botha H. Omental teratoma in supernumerary ovary, in a pregnancy complicated by pre-eclampsia and HIV: case report. Obstetrics and Gynaecology Forum. 2005. Available online: https://journals.co.za/doi/10.10520/EJC73225
- Smith R, Deppe G, Selvaggi S, et al. Benign teratoma of the omentum and ovary coexistent with an ovarian neoplasm. Gynecol Oncol 1990;39:204-7. [Crossref] [PubMed]
- Schmoll HJ. Extragonadal germ cell tumors. Ann Oncol 2002;13:265-72. [Crossref] [PubMed]
- Love RJM. Dermoid cyst simulating gastric ulcer. Br J Surg 1930;18:339-40. [Crossref]
- Judd ES, Fulcher OH. Dermoid cysts of the abdomen. Surg Clin North Am 1933;13:835-42.
- Warfield Jo Jr. Omental dermoid cyst. Am Surg 1956;22:652-6. [PubMed]
- Hogan ML, Barber DD, Kaufman RH. Dermoid cyst in supernumerary ovary of the greater omentum. Report of a case. Obstet Gynecol 1967;29:405-8. [PubMed]
- Printz JL, Choate JW, Townes PL, et al. The embryology of supernumerary ovaries. Obstet Gynecol 1973;41:246-52. [PubMed]
- Ekbladh LE, Fishburne JI. Parasitized dermoid cyst of the omentum. Obstet Gynecol 1973;42:458-60. [PubMed]
- Bell DA, Demopoulos RI. Benign cystic teratoma in the omentum: a mechanism of its development. Diagn Gynecol Obstet 1980;2:205-8. [PubMed]
- Ordóñez NG, Manning JT Jr, Ayala AG. Teratoma of the omentum. Cancer 1983;51:955-8. [Crossref] [PubMed]
- Compton AA, Tandan A, Fleming WP. Coexistent benign teratomas of the omentum and ovary. A case report. J Reprod Med 1985;30:209-10. [PubMed]
- Leno C, Combarros O, Berciano J. Lumbosacral plexopathy due to dermoid cyst of the greater omentum. Postgrad Med J 1987;63:45-6. [Crossref] [PubMed]
- Ralls PW, Hartman B, White W, et al. Computed tomography of benign cystic teratoma of the omentum. J Comput Assist Tomogr 1987;11:548-9. [Crossref] [PubMed]
- Spurney RF, McCormack KM. Immature omental teratoma. Arch Pathol Lab Med 1987;111:762-4. [PubMed]
- Mercer LJ, Toub DB, Cibils LA. Tumors originating in supernumerary ovaries. A report of two cases. J Reprod Med 1987;32:932-4. [PubMed]
- Deppe G, Malviya VK, Jacobs AJ. Extragonadal, mature, solid teratoma with omental implants. A case report. J Reprod Med 1988;33:792-4. [PubMed]
- Drut R, Drut RM, Vollaro F. Mature cystic teratoma of the greater omentum. Pediatr Pathol 1990;10:1033-5. [Crossref] [PubMed]
- Whang SH, Lee KS, Kim PN, et al. Omental teratoma in an adult: a case report. Gastrointest Radiol 1990;15:301-2. [Crossref] [PubMed]
- Besser MJ, Posey DM. Cystic teratoma in a supernumerary ovary of the greater omentum. A case report. J Reprod Med 1992;37:189-93. [PubMed]
- Kriplani A, Takkar D, Karak AK, et al. Unexplained absence of both fallopian tubes with ovary in the omentum. Arch Gynecol Obstet 1995;256:111-3. [Crossref] [PubMed]
- Furuhashi M, Katsumata Y, Oda H, et al. Cystic teratoma of the greater omentum: a case report and review of the literature. J Obstet Gynaecol Res 1997;23:359-63. [Crossref] [PubMed]
- Moon W, Kim Y, Rhim H, et al. Coexistent cystic teratoma of the omentum and ovary: report of two cases. Abdom Imaging 1997;22:516-8. [Crossref] [PubMed]
- Patankar T, Prasad S, Chaudhry S, et al. Benign cystic teratoma of the lesser omentum. Am J Gastroenterol 1999;94:288. [PubMed]
- Ollapallil J, Werapitiya SB, Irukulla S, et al. Benign cystic teratoma of the omentum. ANZ J Surg 2002;72:67-8. [Crossref] [PubMed]
- Pfitzmann R, Klupp J, Krenn V, et al. A dermoid cyst in the greater omentum as a rare epigastric tumor. Z Gastroenterol 2004;42:153-5. [Crossref] [PubMed]
- Yoshida A, Murabayashi N, Shiozaki T, et al. Case of mature cystic teratoma of the greater omentum misdiagnosed as ovarian cyst. J Obstet Gynaecol Res 2005;31:399-403. [Crossref] [PubMed]
- Kubosawa H, Iwasaki H, Kuzuta N, et al. Adenocarcinoma with peritoneal dissemination secondary to multiple mature teratomas of the omentum. Gynecol Oncol 2006;101:534-6. [Crossref] [PubMed]
- Baviskar BP, Dongre SD, Karle RR, et al. Teratoma of lesser omentum in a male infant. J Postgrad Med 2006;52:304-5. [PubMed]
- Chen SS, Chen CP, Chien SC, et al. Spontaneous rupture of omental teratoma mimicking a ruptured ovarian teratoma. Taiwan J Obstet Gynecol 2008;47:229-32. [Crossref] [PubMed]
- Sinha R, Sundaram M, Lakhotia S. Multiple intraabdominal parasitic cystic teratomas. J Minim Invasive Gynecol 2009;16:789-91. [Crossref] [PubMed]
- Ali AA, Sall I, El Kaoui H, et al. Teratoma of the greater omentum. Can J Surg 2009;52:E54-5. [PubMed]
- Wani BN, Rathod V, Banode P, et al. An omental teratoma in a young girl. Clin Pract 2011;1:e129. [Crossref] [PubMed]
- Richardson R, Sharma A, Hammond R. Immature teratoma of the greater omentum. Eur J Obstet Gynecol Reprod Biol 2011;159:478-9. [Crossref] [PubMed]
- Hardesty BM, Ulbright TM, Touloukian C, et al. Primary teratoma of the lesser sac: lesser sac teratoma. Case Rep Oncol Med 2012;2012:604571. [Crossref] [PubMed]
- Sforza M, Andjelkov K, Ivanov D, et al. A rare case of benign omentum teratoma. Srp Arh Celok Lek 2012;140:362-4. [Crossref] [PubMed]
- Schols RM, Stassen LP, Keymeulen KB, et al. Dermoid cyst of the greater omentum: rare and innocent? BMJ Case Rep 2013;2013:bcr2012008304. [Crossref] [PubMed]
- Hegde P. Extragonadal omental teratoma: a case report. J Obstet Gynaecol Res 2014;40:618-21. [Crossref] [PubMed]
- Kim TH, Lee HH. Omental Teratoma Misdiagnosed as Gossypiboma. J Minim Invasive Gynecol 2015;22:709. [Crossref] [PubMed]
- Rampinelli F, Donarini P, Visenzi C, et al. The Rare Extragonadal Omental Teratoma: A Case Report. J Minim Invasive Gynecol 2017;24:1046-8. [Crossref] [PubMed]
- Huang CC, Koh LW. Report: Laparoscopic management for coexistent parasitic ovarian teratoma of the omentum and ovarian mucinous cystadenoma: A case report. Pak J Pharm Sci 2019;32:683-5. [PubMed]
- Sokalska A, Timmerman D, Testa AC, et al. Diagnostic accuracy of transvaginal ultrasound examination for assigning a specific diagnosis to adnexal masses. Ultrasound Obstet Gynecol 2009;34:462-70. [Crossref] [PubMed]
- Alcázar JL, Guerriero S, Laparte C, et al. Diagnostic performance of transvaginal gray-scale ultrasound for specific diagnosis of benign ovarian cysts in relation to menopausal status. Maturitas 2011;68:182-8. [Crossref] [PubMed]
- Huber S, Medl M, Baumann L, et al. Value of ultrasound and magnetic resonance imaging in the preoperative evaluation of suspected ovarian masses. Anticancer Res 2002;22:2501-7. [PubMed]
- Mülayim B, Gürakan H, Dagli V, et al. Unaware of a giant serous cyst adenoma: a case report. Arch Gynecol Obstet 2006;273:381-3. [Crossref] [PubMed]
- Wen KC, Hu WM, Twu NF, et al. Poor prognosis of intraoperative rupture of mature cystic teratoma with malignant transformation. Taiwan J Obstet Gynecol 2006;45:253-6. [Crossref] [PubMed]
- Murawski M, Gołębiewski A, Sroka M, et al. Laparoscopic management of giant ovarian cysts in adolescents. Wideochir Inne Tech Maloinwazyjne 2012;7:111-3. [Crossref] [PubMed]
- Woo Ng Y, Goenadi CJ, Fai Fong Y. Single incision laparoscopic surgery for a large endometriotic cyst. J Surg Tech Case Rep 2013;5:41-4. [Crossref] [PubMed]
- Subbian A, Devi UK, Bafna UD. Accuracy rate of frozen section studies in ovarian cancers: a regional cancer institute experience. Indian J Cancer 2013;50:302-5. [Crossref] [PubMed]
- Kumar AS, Chander V, Parthasarathy J. Diagnostic Accuracy of Intraoperative Frozen Section Analysis in Correlation with Histopathological Diagnosis of Ovarian Tumors in a Tertiary Care Center - A Retrospective Study. Cancer Invest 2021;39:153-8. [PubMed]
- Badru F, Saxena S, Munoz-Abraham AS, et al. Peritoneal Nodules in a Pediatric Patient with Benign Teratoma. A Case Report and Review of Literature. J Pediatr Adolesc Gynecol 2018;31:632-6. [Crossref] [PubMed]
- Huss M, Lafay-Pillet MC, Lecuru F, et al. Granulomatous peritonitis after laparoscopic surgery of an ovarian dermoid cyst. Diagnosis, management, prevention, a case report. J Gynecol Obstet Biol Reprod (Paris) 1996;25:365-72. [PubMed]
- Caspi B, Appelman Z, Rabinerson D, et al. The growth pattern of ovarian dermoid cysts: a prospective study in premenopausal and postmenopausal women. Fertil Steril 1997;68:501-5. [Crossref] [PubMed]
- Cohen A, Almog B, Tulandi T. Sclerotherapy in the management of ovarian endometrioma: systematic review and meta-analysis. Fertil Steril 2017;108:117-24.e5. [Crossref] [PubMed]
- Koc S, Tapisiz OL, Turan T, et al. Malignant transformation of mature cystic teratoma of the ovary: a case series. J Exp Ther Oncol 2015;11:11-6. [PubMed]
- Singh N, Baby D, Rajguru JP, et al. Inflammation and cancer. Ann Afr Med 2019;18:121-6. [Crossref] [PubMed]
- Saleh M, Bhosale P, Menias CO, et al. Ovarian teratomas: clinical features, imaging findings and management. Abdom Radiol (NY) 2021;46:2293-307. [Crossref] [PubMed]
Cite this article as: Li T, Zhang W, Huang J, Shen Y, Cui T, Giannini A, Tapisiz OL, Lasmar RB, Lasmar BP. Rare multiple teratomas of the omentum and giant fused teratomas of the bilateral ovaries: a case report and review of the literature. Gynecol Pelvic Med 2021;4:29.



