
Mesh vaginal colpopexy complications analysis—multicenter study results
Introduction
Disappointment in the results of surgical self-tissue treatment [high risk of recurrent pelvic prolapse, requiring 30% of reoperations (1)] led to the rapid introduction of mesh technologies in genital prolapse surgery. The abdominal (laparoscopic or robot assisted) surgical approach for POP is the standard but it required longer operation time, longer recovery, longer learning curve and higher cost (1,2). Therefore, vaginal mesh surgery was attracted as a minimally invasive surgery with good anatomical results (3). Vaginal mesh devices were developed apace at period from 2004 to 2008. More than 100 synthetic mesh kits were available for surgeons. This scenario increases the risk of complications and in some cases, it can be very serious. Surgeons were inspired by favorable shot-term results. Unfortunately, there is still no consensus how to treat and diagnosed mesh-related complications (4). This is responsible for market withdrawal of many vaginal kits. This was the reason for market withdrawal of many vaginal kits and in 2014 the FDA required to reclassify transvaginal mesh as high risk (class III) medical devices. It would require manufactures to provide clinical data in premarket approval application to support the safety and effectiveness of vaginal mesh (5,6).
Mesh-related complications, developing after pelvic organ prolapse vaginal correction using synthetic mesh are widely discussed by surgeons recently. To study the structure of complications, multicenter retrospective studies are carried out on the safety and effectiveness of using mesh (7,8). According to Jacquetin and Cosson, severity of that complications is frequently overestimated. In June 2009, Terminology and Classification of Complications was proposed for approval by IUGA (International Urogynecological Association) (9). DeLancey, Hurtado and Appell in their articles detailed complications, requiring complete removal of the mesh, whose number is steadily increasing (10,11). The purpose of our study was to assess the number of complications (mesh-related and surgical), to determine the way of prevention and treatment complications and describe the most severe and rare of them.
We present the following article in accordance with the STROBE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-19/rc).
Methods
Our transvaginal Russian group decided to analyze complications’ appearance in women, who underwent pelvic organ prolapse surgery using Gynecare ProliftTM system during 3 years within 7 major clinics of Moscow and Moscow Region. There was a total of 421 interventions, 216 of which were Prolift anterior, 33—Prolift posterior, 142—Prolift total, 30—Prolift anterior with posterior. Patients, who underwent mesh repair had symptomatic prolapse with POP-Q stage 2–4. The surgical procedure was standardized to using a trocar-guided transvaginal mesh kit.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics committee of Moscow Regional Scientific Research Institute of Obstetrics and Gynecology (No.: 06004245) and informed consent was taken from all individual participants.
Complications were divided into three main groups: intraoperative, postoperative, mesh-related.
Structure of intraoperative complications is represented in Table 1.
Table 1
| Intraoperative complications | n | 5.8% |
|---|---|---|
| Urethral injury | 2 | 0.5% |
| Urine bladder injury | 7 | 1.7% |
| Rectal injury | 4 | 1% |
| Massive bleeding (>500 mL) | 12 | 2.6% |
There were 6 incidents of intraoperative urine bladder injury, which were sutured afterward and 2 of them led to anterior colporrhaphy instead of a mesh using during colpopexy. In 1 case bladder injury was revealed only on the 7th day after intervention, when hematuria was escalated (Figure 1). During cystoscopy bladder’s defect with part of the mesh was revealed. Thereafter, fistula with a piece of the prosthesis was excised and then wound closure was performed. All patients underwent intermittent catheterization up to 3–7 days. The postoperative period was uneventful.
It should be noted that the capability to perform cystoscopy and ureteral catheter or stent placement are beneficial skills in the diagnosis and prevention of complications.
The rectal injury occurred in 4 cases and all of them were during dissection between the vaginal wall and fascia. After the closure of the defect, mesh was inserted only in 2 of them. The other two cases ended by performing colpoperineorraphy. The postoperative period was uneventful. The decision on the use of a synthetic mesh after injury closure is decided by surgeons ambiguously. There are no such criteria nowadays.
In almost all cases of moderate bleeding (n=12), vessels were found and ligated intraoperatively by vaginal approach. In 1 case of blood loss amount of 1,000 mL, the source was the left gluteal artery. Also, we observed the occurrence of bleeding from paraurethral venous plexus with hematoma formation in Retzius and retroperitoneal spaces. In that case, laparotomy was performed, after revision and sanitation, sacrocolpopexy was performed following vaginal mesh excision. One fatal outcome was due to massive bleeding that caused emergency laparotomy with internal iliac artery ligation.
Postoperative complications were in 59 cases, their structure detailed in Table 2.
Table 2
| Postoperative complications | n | 14% |
|---|---|---|
| Febrile and above fever (>38 °C) | 11 | 2.6% |
| Obstructive urination | 14 | 3.3% |
| Clinically significant vaginal hematomas | 23 | 5.5% |
| Clinically significant perineal hematomas | 11 | 2.6% |
Obstructive urination usually resolved at 3–5th day after surgery. During that days intermittent catheterization of urine bladder administered to patients.
In more detail, we would like to point on the hematomas of the vagina and perineum, which are observed in almost all patients who have undergone Prolift colpopexy. Small hematomas, which were detected by ultrasound, resolved completely, without affecting the course of the postoperative period. Larger hematomas (more than 100 mL) in 10 cases festered, were punctured and followed by antibiotic therapy. Only in 1 case, after 6 months, the removal of the mesh (Prolift posterior) was required due to severe pain in the perineum and infection of synthetic material.
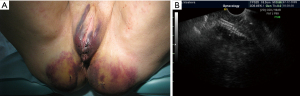
Subcutaneous hematomas of the perineum, buttocks and the posterior surface of thigh always had a frightening appearance, but they all resolved without the use of additional therapy (Figures 2,3).
Mesh-related complications observed in 40 cases, which were (Table 3).
Table 3
| Mesh-related complications | n | 9.5% |
|---|---|---|
| Posterior vaginal wall erosion | 16 | 3.8% |
| Infection of the synthetic mesh with formation of abscess or phlegmons | 3 | 0.7% |
| Mesh shrinking with deformation of the vagina | 5 | 1.2% |
| Perineal or buttock pain | 16 | 3.8% |
In our study, we considered surgically treated erosions only. Small diameter erosions (<1 cm2) were treated conservatively with local estrogen application and were fully resolved.
Bigger erosions excised within healthy tissue borders along with mesh, the wound was sutured and in almost all cases subsequently healed.
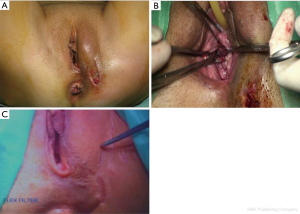
Erosion recurrence appeared only in 2 cases, which required complete excision of the mesh because of its infection (Figure 4).
Mesh infection with formation of abscess appeared due to long-term erosions (portal of entry). Women complained about severe pain and purulent discharge in 2 cases at 4 and 6 weeks after intervention. Bimanual and ultrasound examination showed posterior vaginal wall abscess presence, the mesh was completely excised, wound healing process was uneventful.
Below is a clinical example of the pelvic phlegmon formation in a 37-year-old patient after Prolift anterior & posterior colpopexy, urethropexy by TVT-O procedure for II grade pelvic organ prolapse with stress urinary incontinence. A month later after the surgery, the patient required readmission for generalized infection and abscessing purulent phlegmon of the left buttock (Figure 5A). Cultural growth identified Staphylococcus aureus. The affected area was opened and drained, the patient received the full range of necessary treatment without significant improvement. A thorough examination of the vaginal mucosa (this was possible only under general anesthesia) revealed extensive erosion of the anterior vaginal wall, which served as the portal of entry of the infection (Figure 5B). The mesh was immediately excised. The TVT-O sling under the middle third of the urethra remained intact and, thereafter, wasn’t removed. After 6 months patient Six months later, the patient again complained of dyspareunia; vaginal examination revealed recurrent erosion of the anterior vaginal wall, which required another (fourth!) surgical intervention with the secondary closure of the wound (Figure 5C). At the present day, after so many interventions, the patient is being a healthy, continent and has pelvic organ prolapse absence.
Mesh shrinkage was also referred to as mesh-related complications. Studies observing mesh shrinkage in rats after anterior abdominal wall implantation of the synthetic mesh resulted in up to 40% reduction of its primary measurements. It’s often reduced in size without any symptoms. Nevertheless, our study observed 5 cases of mesh shrinkage followed by continuous or intermittent pain and significant vaginal shortening (in one case almost to 2 cm) (Figure 6). In 2 cases mesh was particularly excised with secondary pelvic organ prolapse correction laparoscopically (sacrocolpopexy).
Statistical analysis
This was a descriptive study and standard statistical analyses were performed. Categorical data were presented as % (n/N) and continuous data were presented as mean ± standard deviation or median (range). All data was analyzed with Microsoft Excel 2019 (Microsoft Corporation, Redmond, USA).
Conclusions
It should be noted that surgery for complete removal of the prosthesis is an intervention of increased complexity with a high risk of bladder and rectal injury. Such operations should be performed only in highly specialized clinics that are positioning as reference centers of these complications. Therefore, we cannot consider extraperitoneal colpopexy using the Prolift system as a minimally invasive intervention and propose this operation as a routine method.
Based on the lessons learned, we have identified priority indications for surgery (senile and elderly patients with complete prolapse of the uterus and vaginal walls, recurrent forms of genital prolapse) and contraindications (sexually active patients with pelvic organ prolapse II–IV stages. In our group, erosions appeared mainly in patients aged 37 to 50 years). Reduce of concomitant hysterectomies amount and perioperative local estrogen administration significantly improve surgery outcomes. It should be noted that the operation should not be aimed at cosmetic results only. The success of the intervention directly depends on strict adherence to the indications and contraindications for vaginal mesh colpopexy in patients with genital prolapse. Patients who experience various types of complications after surgical correction of genital prolapse using mesh should be referred for treatment only to highly specialized institutions that are deeply engaged in this problem.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Surgical Treatment of Genital Prolapse and Urinary Incontinence”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-19/rc
Data Sharing Statement: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-19/dss
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-19/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-21-19/coif). The series “Surgical Treatment of Genital Prolapse and Urinary Incontinence” was commissioned by the editorial office without any funding or sponsorship. AP served as an unpaid Guest Editor of the series and serves as an unpaid editorial board member of Gynecology and Pelvic Medicine from August 2020 to July 2022. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics committee of Moscow Regional Scientific Research Institute of Obstetrics and Gynecology (No.: 06004245) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 2013;CD004014. [PubMed]
- Lucot JP, Cosson M, Bader G, et al. Safety of Vaginal Mesh Surgery Versus Laparoscopic Mesh Sacropexy for Cystocele Repair: Results of the Prosthetic Pelvic Floor Repair Randomized Controlled Trial. Eur Urol 2018;74:167-76. [Crossref] [PubMed]
- Diwadkar GB, Barber MD, Feiner B, et al. Complication and reoperation rates after apical vaginal prolapse surgical repair: a systematic review. Obstet Gynecol 2009;113:367-73. [Crossref] [PubMed]
- Karmakar D, Hayward L. What can we learn from the vaginal mesh story? Climacteric 2019;22:277-82. [Crossref] [PubMed]
- Unger CA, Barber MD. Vaginal Mesh in Pelvic Reconstructive Surgery: Controversies, Current Use, and Complications. Clin Obstet Gynecol 2015;58:740-53. [Crossref] [PubMed]
- US Food and Drug Administration. Proposed order: reclassification of surgical mesh for transvaginal pelvic organ prolapse repair and surgical instrumentation for urogynecologic surgical mesh procedures; designation of special controls for urogynecologic surgical mesh instrumentation. 2014. Available online: https://www.federalregister.gov/articles/2014/05/01/2014-09907/reclassification-of-surgical-mesh-for-transvaginal pelvic-organ-prolapse-repair-and-surgical. Accessed January 30, 2015.
- Bako A, Dhar R. Review of synthetic mesh-related complications in pelvic floor reconstructive surgery. Int Urogynecol J Pelvic Floor Dysfunct 2009;20:103-11. [Crossref] [PubMed]
- Abdel-Fattah M, Ramsay IWest of Scotland Study Group. Retrospective multicentre study of the new minimally invasive mesh repair devices for pelvic organ prolapse. BJOG 2008;115:22-30. [Crossref] [PubMed]
- Jacquetin B, Cosson M. Complications of vaginal mesh: our experience. Int Urogynecol J Pelvic Floor Dysfunct 2009;20:893-6. [Crossref] [PubMed]
- Hurtado EA, Appell RA. Management of complications arising from transvaginal mesh kit procedures: a tertiary referral center's experience. Int Urogynecol J Pelvic Floor Dysfunct 2009;20:11-7. [Crossref] [PubMed]
- Margulies RU, Lewicky-Gaupp C, Fenner DE, et al. Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol 2008;199:678.e1-4. [Crossref] [PubMed]
Cite this article as: Popov A, Abramyan K, Klyushnikov I, Kasyan G. Mesh vaginal colpopexy complications analysis—multicenter study results. Gynecol Pelvic Med 2022;5:3.






