Vascular complication during staging lymphadenectomy in early-stage ovarian cancer
Introduction
Ovarian cancer (OC) is the fifth most frequent female cancer and represents the main cause of death from gynecological cancer (1). In 70% of cases, OC may be diagnosed at an advanced stage with nonspecific symptoms (2). In early-stage OC, surgical staging is necessary. According to the National Comprehensive Cancer Network, surgical staging includes total hysterectomy, bilateral salpingo-oophorectomy, omentectomy, peritoneal biopsies, and pelvic and lumboaortic lymphadenectomy (3).
Staging surgery should be performed through a vertical midline abdominal incision. Nevertheless, in specialized centers, staging surgery may be performed through laparoscopic approach in selected cases (3). Minimally invasive surgery is associated with a lower blood loss, shorter hospital stay, better quality of life, and fewer major complications compared to classic open surgery (4-7).
Nonetheless, if laparoscopy is performed, when major complications occur during this procedure, rapid life-saving treatments could be necessary alongside good surgical skills.
We present a 63-year-old woman case with a 55 mm, multilocular-solid left adnexal mass, Color Score 2, with abnormal CA 125. Adnex model suggested for a malignant lesion (8). No distant metastatic localizations have been identified on computed tomography. The frozen section analysis of the left adnexa showed a high-grade serous OC, thus surgical staging was performed.
This article aims to show a possible and dangerous vascular complication that may occur during pelvic lymphadenectomy for OC surgical staging.
Operative technique
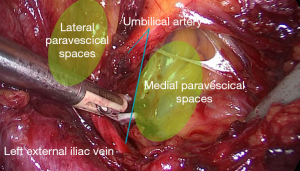
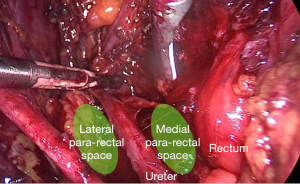
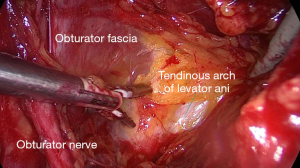
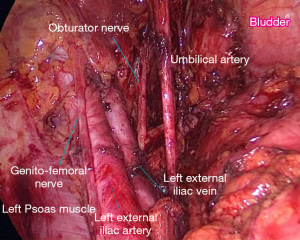
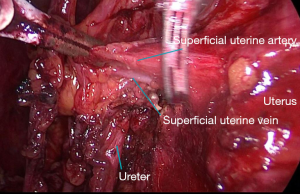
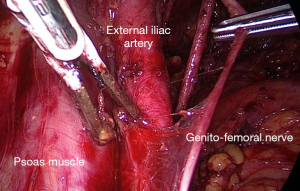
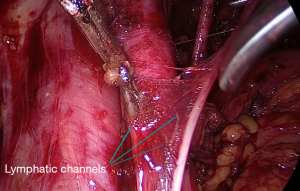
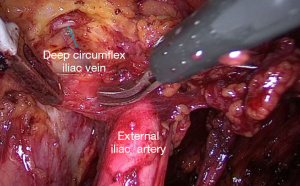
(I) Develop the paravesical and pararectal spaces to gain a good exposure of the surgical field (Figures 1-3). (II) Furthermore, the main anatomical structures should be identified: ureter, obturator nerve, uterine vessels, umbilical artery (Figures 4,5). (III) Perivascular lymphatic tissue should be dissected for systematic removal of the pelvic lymph nodes, paying attention to not injure the genito-femoral nerve (Figures 6,7). The lower limit of pelvic lymphadenectomy is represented by the deep iliac circumflex vein (Figure 8).
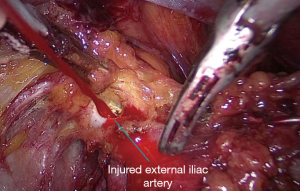
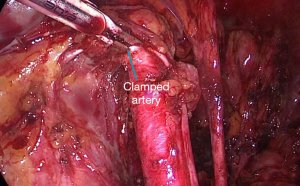
(IV) In case of accidental vascular injury, a quick clamping of the vessel must be promptly performed (Figures 9,10). The assistant must move the camera away and keep a correct view of the entire surgical field, preventing the optics from getting soiled with blood.
(V) Once the bleeding has been stopped, better exposure of the vessel could be necessary before applying the suture’s stitches. The repair of the vessel can take place both in laparoscopy and in laparotomy (9). In our case, a median longitudinal sub-navel incision was made and the artery was repaired with two 3-0 Vicryl stitches. Thanks to the rapid intervention, the patient had an estimated total blood loss of 1,200 milliliters (Video 1).
Comments
International guidelines recommend OC treatment in referral centers with dedicated gynecologists with expertise in gynecologic oncology (3). Accidental internal iliac artery injury may require life-saving interventions. When complications occur during minimally invasive surgery, the surgeon’s surgical skills are essential for quick and correct management of the hurdle.
Nowadays, a specific consensus regarding the best surgical approach to adopt when managing possible complications is still missing (10). The surgeon should always use his/her most comfortable and confident surgical approach (11).
Taking this scenario into account, we strongly believe that it’s essential for these surgeries to take place in a cancer center and to be performed by highly skilled and dedicated surgeons.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Laparoscopic Surgery for Ovarian Cancer”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.org/article/view/10.21037/gpm-20-26/coif). The series “Laparoscopic Surgery for Ovarian Cancer” was commissioned by the editorial office without any funding or sponsorship. VAC served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this study and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Torre LA, Trabert B, DeSantis CE, et al. Ovarian cancer statistics, 2018. CA Cancer J Clin 2018;68:284-96. [Crossref] [PubMed]
- Doubeni CA, Doubeni AR, Myers AE. Diagnosis and Management of Ovarian Cancer. Am Fam Physician 2016;93:937-44. [PubMed]
- National Comprehensive Cancer Network. Ovarian cancer. (Version 32019). Available online: http//www.nccn.org/professionals/physician_gls/pdf/ovarian.pdf
- Gueli Alletti S, Capozzi VA, Rosati A, et al. Laparoscopy vs. laparotomy for advanced ovarian cancer: a systematic review of the literature. Minerva Med 2019;110:341-57. [Crossref] [PubMed]
- Capozzi VA, Sozzi G, Gambino G, et al. Laparoscopy versus laparotomy for surgical treatment of obese women with endometrial cancer: A cost-benefit comparative analysis. Mol Clin Oncol 2019;11:335-42. [PubMed]
- Cianci S, Tarascio M, Rosati A, et al. Sexual function and quality of life of patients affected by ovarian cancer. Minerva Med 2019;110:320-9. [Crossref] [PubMed]
- Uccella S, Zorzato PC, Lanzo G, et al. The role of sentinel node in early ovarian cancer: a systematic review. Minerva Med 2019;110:358-66. [Crossref] [PubMed]
- Van Calster B, Van Hoorde K, Froyman W, et al. Practical guidance for applying the ADNEX model from the IOTA group to discriminate between different subtypes of adnexal tumors. Facts Views Vis Obgyn 2015;7:32-41. [PubMed]
- Krishnakumar S, Tambe P. Entry complications in laparoscopic surgery. J Gynecol Endosc Surg 2009;1:4-11. [Crossref] [PubMed]
- Samsonov VT, Ermolov AS, Gulyaev AA, et al. Laparoscopy in emergency abdominal surgery. Khirurgiia (Mosk) 2019;32-7. [Crossref] [PubMed]
- Capozzi VA, Rosati A, Turco LC, et al. Surgery vs. chemotherapy for ovarian cancer recurrence: what is the best treatment option. Gland Surg 2020; [Crossref]
Cite this article as: Capozzi VA, Armano G, Ceni V, Riccò M, Volpe N, Berretta R. Vascular complication during staging lymphadenectomy in early-stage ovarian cancer. Gynecol Pelvic Med 2020;3:23.