Risk of ureteric injury during ipsilateral uterosacral ligament vault suspension with intra-operative cystoscopy
Introduction
Post hysterectomy vaginal vault prolapse (PHVVP) occurs in up to 40% of women (1) following hysterectomy with 6–8% of cases requiring surgery (2). The incidence of PHVVP is up to five times higher when the hysterectomy is performed for uterovaginal prolapse compared to other indications (3). PHVVP often significantly impacts quality of life with associated vaginal discomfort as well as bowel, bladder and sexual dysfunction. Risk factors for PHVVP include advanced age, obesity, previous vaginal delivery, post-menopausal status, genetic predisposition and connective tissue disorders (4).
Knowledge of the anatomical structures which support the vagina is essential to understand why hysterectomy predisposes to vaginal prolapse. DeLancey (5) described this support at three levels. The upper quarter is suspended by the cardinal and uterosacral ligament. The middle two quarters by attachment to the arcus tendinous fascia anteriorly and posteriorly to the pubococcygeus and iliococcygeus fascia. Finally, the lower quarter of the vagina is maintained by fusion to the urogenital diaphragm anteriorly and the perineal body posteriorly. Additional support is provided by the pubocervical fascia anteriorly and the rectovaginal fascia posteriorly. The necessary detachment of the vaginal apex from the supporting cardinal/uterosacral ligament complex during hysterectomy predisposes to PHVVP.
Unsurprisingly given the risk of PHVVP, many recommend that a preventative procedure is performed at the time of hysterectomy. Multiple procedures are described including vaginal surgeries such as uterosacral ligament vault suspension (ULVS), sacrospinous ligament fixation and Moschowitz closure of the Pouch of Douglas, open procedures and more recently laparoscopic procedures such as sacrocolpopexy and uterosacral plication (1).
Modified McCall’s culdoplasty is a ULVS procedure which involves re-attaching the uterosacral ligament to the ipsilateral peritoneal side of the vaginal vault and is a widely advocated method for the prevention of PHVVP. Compared to sacrospinous fixation, it is associated with reduced blood loss, reduced operating time, a lower failure rate and has the added benefit of increasing the vaginal length as well as maintaining the normal vaginal alignment (6-8). Furthermore, ULVS is more effective than other techniques such as a Moschowitz closure of the Pouch of Douglas in the prevention of PHVVP (9).
However, a justified concern of ULVS is the risk of ureteric injury either directly or via obstruction secondary to ureteric kinking. Several studies have been performed investigating outcomes from ULS (10-17). Collective weaknesses of these studies include small sample sizes and the absence of a robust method for identifying ureteric injury. This paper describes our experience of 127 consecutive cases of transvaginal ULVS with the routine use of intra-operative cystoscopy with indigocarmine dye to reliably detect ureteric injury.
Methods
A retrospective observational study was performed detailing outcomes from vaginal surgical procedures with transvaginal ULVS performed routinely during vaginal vault closure. All procedures were carried out in a single UK hospital by the senior author.
In all cases ULVS was performed alongside a primary procedure of either a vaginal hysterectomy (VH) with bilateral salpingo-oophorectomy (BSO) or a vaginal bilateral salpingo-oophorectomy (VBSO) in patients who had previously undergone a hysterectomy. Indications for surgery included endometriosis, menorrhagia, abnormal uterine bleeding and PHVVP. The ovaries were removed either prophylactically at the time of hysterectomy or due to post hysterectomy pain due to “trapped ovary syndrome.”
Data collection involved review of the case notes for all ULVS procedures performed over a 4-year period (February 2010 and July 2014). One hundred and forty two women initially met inclusion criteria. Exclusion criteria were women with incomplete data available after case note review (n=15). Data was collected on patient age, body mass index (BMI), comorbidity, previous pelvic surgery, parity, menopausal status and indication for surgery. The primary outcome measure was the incidence of ureteric injury or obstruction. Secondary outcome measures included duration of operation, length of hospital stay, change in haemoglobin concentration between the preoperative value and the first post-operative day, surgical complications and histology. Post-operative infections were included as complications if antibiotics were received and excessive blood loss was included if blood transfusion was required.
The surgical protocol ensured all patients received a single dose of intra-operative intravenous antibiotics. Post-operatively, patients wore thrombotic deterrent stockings and received subcutaneous low molecular weight heparin whilst in hospital unless there were contraindications. Early discharge was facilitated where possible through an enhanced recovery program. Patients were routinely followed up 2–3 months post-operatively in clinic.
The surgical technique is described as follows with the patient positioned in lithotomy throughout: Once the VH (with or without BSO) has been undertaken by standard methodology, a large roll gauze swab was inserted in the pouch of Douglas to pack the bowels away. The uterosacral ligament on the left side was put under tension at a 45 degree angle and palpated to ascertain its reliability and strength. An illuminating retractor (Myaski) was introduced in the pelvis to retract the rectum medially and to visualise the uterosacral ligament. A set of three PDS (polydioxanone; Ethicon) size No1 sutures were placed into the ligament; the most caudal is placed below the ischial spine, the upper is placed just above the ischial spine and the middle is placed in-between (this is to avoid ureteric injury and constriction of the pouch of Douglas). The same process was repeated on the contralateral uterosacral. The first cystoscopy was then performed to identify ureteric injury (ureteric transfixion or entanglement). All the sutures were then re-sutured to the vaginal vault which will close the vault and suspend it. At this point a second cystoscopy was performed and the swab was removed before the vault was closed by tying all the sutures. The third and final cystoscopy was then performed after tying sutures, primarily to check for kinking of the ureter which may occur during suture tying.
In patients who have previously had a hysterectomy the technique differed from above as follows: The vaginal scar of the previous hysterectomy is excised to allow entry or access to the pouch of Douglas. A moist abdominal pack is then placed in the pelvis to pack the bowels away. A tension suture is inserted at 5 and 7 o’clock through the vaginal vault which would also include the caudal end of the uterosacral ligament; a traction is applied to this suture at 45º direction to place the uterosacral ligament under tension and palpable so that its integrity and strength are assessed. An illuminated retractor was then introduced and all adhesions from previous surgery are divided by sharp dissection under direct vision. Once the tubes and ovaries are removed; a set of three sutures are inserted in the uterosacral ligament as described above.
Intra-operative cystoscopy with indigocarmine (Indigotridisulfonate sodium) dye was used during in all cases as it increases detection rates of ureteric injury from 50% to 80–90% and bladder injury from 25% to 80% (18). The cystoscopy was performed as follows: firstly, 3–4 mL of dye was administered to the patient intravenously immediately prior to cystoscopy. Indigo carmine is known to be safe (19) and has a half-life of 4–5 minutes with predominately renal excretion. It is usually present in urine 5–10 minutes after injection. A 70-degree cystoscope is then introduced into the bladder to visualise efflux of urine through both ureteric orifices. Failure to visualise the dye thirty minutes after injection warrants further investigation of ureteric patency with an intravenous pyelogram or retrograde ureteropyelogram (18) and/or uterosacral suture removal if there is a concern regarding ureteric kinking.
Statistical analysis was performed using standard statistical techniques. Statistical significance was determined using the two tailed t-test. P<0.05 was considered statistically significant for all comparisons. Ethical approval was not required for this study as it was retrospective case series.
Results
One hundred and forty two consecutive cases of modified McCall’s culdoplasty met initial inclusion criteria. One hundred twenty-seven (90%) had complete data sets available and were analysed. One hundred and nine of these cases involved VH with BSO and 18 cases involved a VBSO without hysterectomy (hysterectomy having already been performed in these cases). ULVS was performed in all cases.
Table 1 details the patient group characteristics. The majority of patients were multiparous, post-menopausal and had undergone previous pelvic surgery. Indications for surgery are detailed in Table 2. The most common indication was uterovaginal prolapse (71.7%).
Table 1
| Characteristic | All procedures (n=127) |
|---|---|
| Age (year) | |
| Mean | 54.2 |
| Range | 36–83 |
| Parity | |
| Multiparous | 122 (96.1%) |
| Nulliparous | 5 (3.9%) |
| Range | 0–7 |
| Body mass index (BMI) | |
| Mean | 29.4 |
| Range | 21–44 |
| Post-menopausal | 71 (55.9%) |
| Previous pelvic surgery | 67 (52.8%) |
All procedures include both VH with BSO with ULVS and VBSO with ULVS. VH, vaginal hysterectomy; BSO, bilateral salpingo-oophorectomy; ULVS, uterosacral ligament vault suspension; VBSO, vaginal bilateral salpingo-oophorectomy.
Table 2
| Indication | VH + BSO (n=109) (%) | Vaginal BSO (n=18) (%) | Combined (n=127) (%) |
|---|---|---|---|
| Vaginal wall prolapse | 72 (67.0) | 17 (94.4) | 89 (70.1) |
| HMB | 22 (20.2) | 0 | 22 (17.3) |
| Uterine fibroids | 4 (3.7) | 0 | 4 (3.1) |
| FH of ovarian malignancy | 1 (0.9) | 0 | 1 (0.8) |
| Chronic pelvic pain | 6 (5.5) | 1 (5.6) | 7 (5.5) |
| PMB | 2 (1.8) | 0 | 2 (1.6) |
Within the 7 cases of chronic pelvic pain there were 4 cases of endometriosis, 1 case of adenomyosis, 1 case of severe pelvic inflammatory disease with endometriosis and 1 case of “trapped ovary syndrome”. VH, vaginal hysterectomy; BSO, bilateral salpingo-oophorectomy; HMB, heavy menstrual bleeding; FH, family history; PMB, post-menopausal bleeding.
The outcomes following surgery are detailed in Table 3. The overall complication rate was 7.1%. There was a single case of direct ureteric injury giving a ureteric injury rate of 0.8%. This injury occurred during the religation of the uterine artery pedicle to secure haemostasis whilst performing the hysterectomy. This injury was identified intra-operatively from cystoscopy allowing successful repair via laparotomy. There was no long term morbidity reported from this case. This series did not demonstrate any cases of ureteric obstruction due to kinking of the ureter.
Table 3
| Outcome | VH + BSO (n=109) | Vaginal BSO (n=18) | Combined (n=127) |
|---|---|---|---|
| Operation completed via vaginal route | 108 (99.1%) | 18 (100%) | 126 (99.2%) |
| Mean operating time (min) | 192 | 182 | 189 |
| Post-operative hospital stay (days) | |||
| Mean | 2.65 | 2.72 | 2.68 |
| Range | 1–6 | 1–8 | 1–8 |
| Mean decrease in Hb g/L | 2.47 | 2.35 | 2.44 |
| Benign histology | 108 (99.1%) | 18 (100%) | 127 (100%) |
| Complications | |||
| Ureteric injury/obstruction | 1 | 0 | 1 (0.8%) |
| Infection | 1 | 0 | 1(0.8%) |
| Haemorrhage with transfusion | 4 | 0 | 4 (3.1%) |
| Return to theatre | 1 | 0 | 1 (0.8%) |
| ACS | 1 |
Haemoglobin (Hb) change between pre-operatively and 1st post-operative day. Failure to pass urine following removal of the catheter post operatively is a relatively common complication not included in the above table. VH, vaginal hysterectomy; BSO, bilateral salpingo-oophorectomy; ACS, acute coronary syndrome.
The most common complication in this series was blood loss requiring transfusion which accounted for 50% (4 cases) of complications. However, in 3 out of these 4 patients the pre-operative haemoglobin was suboptimal, being less than 10.5 g/L, meaning these patients were more susceptible to post-operative anaemia even without excessive blood loss. There was a single patient who returned to theatre in the post-operative period due to inadequate haemostasis from the uterine vascular pedicle which required resuturing. There were no bowel or bladder injuries, no intensive care admissions and no deaths.
The surgery was completed via the vaginal route in 99.2% of the women (126/127). There was a single case of conversion to laparotomy to complete the procedure. Over the entire 4-year period, 18.2% of patients were discharged on the first post-operative day and 47.2% on the second day. However, when analysing cases from the final year of data collection (n=29), the figures are 58.6% and 93.1% respectively which is likely to represent a staff learning curve and experience with the principles of enhanced recovery. The uterine histology was benign in all except one case where an unexpected endometrial malignancy was found. The mean specimen weight was 121.8 g with a range of 30–441 g.
Discussion
McCall first published his description of a transvaginal culdoplasty technique to support the vaginal vault following VH in 1957 (20). Since then, numerous studies using modified versions of this procedure have demonstrated benefit in the prevention and treatment of PHVVP (8,9,21,22). Therefore, many recommend ULVS is performed routinely during hysterectomy (18) despite studies finding it to be a statistically significant risk factor for perioperative complications, especially ureteric obstruction (23).
The results of this study suggest ULVS is a safe additional procedure to perform at the time of VH to prevent PHVVP. The single ureteric injury that occurred in this series was unrelated to the ULVS part of the procedure, but if included gives an injury rate of 0.8%. This compares favourably with previous estimates of the ureteric injury rate following ULVS which range from 0.6–10.9% (10-16,24) and is similar to the incidence of urinary tract injuries from all types of gynaecological surgery [0.2 to 15 per 1,000 cases (18)].
There are two previous studies (1,25) which involve the routine use of cystoscopy with indigocarmine dye allowing the closet comparison to this series. Niblock and colleagues (1) demonstrated a single case of ureteric obstruction and no direct ureteric injuries in 70 cases of VH with ULVS. As in this study, the routine use of cystoscopy allowed intra-operative detection and correction of the problem avoiding significant morbidity. Aronson and colleagues (25) described a ureteric injury rate of 0.24% in a series of 411 patients undergoing ULVS with cystoscopy and indigo carmine. The authors advocated placing the uterosacral sutures deeper posteriorly and less cephalad to reduce the risk of ureteric injury.
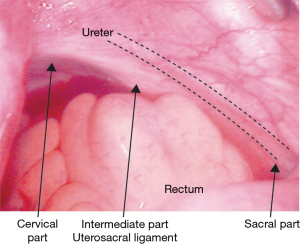
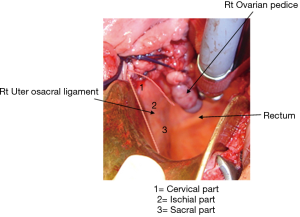
Consideration of the anatomy of the uterosacral ligaments and their relationship to the ureters may explain some of the observed variation in the ureteric injury rate. The uterosacral ligaments are two bands of fibroelastic and smooth muscle tissue which run from the sacrum (presacral fascia and first four sacral vertebrae) to the posterior aspect of the cervix and upper vagina. The ureters run lateral to the uterosacral ligaments beneath the peritoneum of the pelvic side wall descending anteromedially into the pelvis (Figure 1).
Previous authors (6,26) have described the proximity of different parts of the uterosacral ligaments to the ureter. There is an average 1.4 cm distance at the cervix and a larger 4.1 cm (±0.6 cm) distance at the level of the sacrum with a more variable 4.9 cm (±2 cm) distance at the level of the ischial spines. Based on this the authors recommend the intermediate part of the uterosacral ligament as the safest site to place suspension sutures (Figures 1,2). Although the cervical portion of the uterosacral ligament is often the most accessible for suspension sutures it is likely to represent the highest risk.
An inexperienced surgeon, higher BMI, increased uterine size, extra-uterine pathology, blood loss over 800 mL and a longer procedure increase the likelihood of ureteric injury (18,27). With specific regard to ureteric injury during ULVS, a concomitant anterior repair procedure increases the risk of ureteric injury and the use of a suture-capturing device for suspension suture placement reduced the risk of injury (28).
However, the ureters are at risk of injury or kinking during vault suspension procedures even with the most cautious surgical technique by an experienced surgeon. Occult ureteric injury or obstruction is relatively common resulting in a delayed diagnosis often by several weeks. This delay can lead to significant morbidity including chronic infection, urinary incontinence, ureteric fistula formation and even the loss of the connected kidney (27). Intra-operative diagnosis is desirable as early recognition and repair of ureteric injury reduces post-operative complications, overall morbidity and the need for repeat operations.
The use of cystoscopy with indigocarmine dye represents a robust method for identifying ureteric injury intra-operatively. The sensitivity and specificity are 94.4% and 99.5% respectively, with reassuringly low false positive and false negative rates at 0.4% and 0.3% respectively (24). The complication rate from cystoscopy itself is extremely low with post-operative infection being the most common. It is also a relatively quick and simple procedure to perform during the operation. Therefore, the authors of this study recommend it is used routinely during hysterectomy with ULVS.
In this series the overall complication rate was 7.1% with bleeding requiring blood transfusion being the most common. It is likely that by attempting to optimise these patients pre-operatively with investigation and treatment for anaemia the blood transfusion rate could have been reduced. Furthermore, there was no excessive bleeding reported from performing the McCall’s culdoplasty part of the procedure and in these cases the majority of the blood loss occurred during the hysterectomy part of the procedure.
Limitations of this study include the fact that the patient group were selected from a single gynaecological unit and all operations were performed by a single surgeon limiting application of these findings to the wider population. However, the age, parity and levels of co-morbidity of patients in this study were comparable to other studies suggesting they may be applicable. Other limitations include the retrospective nature of the study and the three month maximum follow up period meaning long term outcomes were not determined.
In conclusion, ULVS represents a feasible and safe procedure for the prevention of PHVVP with a low rate of ureteric obstruction or injury. However, given the anatomical proximity of the ureter to the uterosacral ligament the authors recommend that intra-operative cystoscopy with indigocarmine dye should be used routinely as a simple method to identify ureteric injury or obstruction allowing immediate correction.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.org/article/view/10.21037/gpm-20-12/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval was not required for this study as it was retrospective case series and no patient identifiable information was used.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Niblock K, Bailie E, McCracken G, et al. Vaginal McCall culdoplasty versus laparoscopic uterosacral plication to prophylactically address vaginal vault prolapse. Gynecol Surg 2017;14:3. [Crossref] [PubMed]
- Aigmueller T, Dungl A, Hinterholzer S, et al. An estimation of the frequency of surgery for post hysterectomy vault prolapse. Int Urogynecol J 2010;21:299-302. [Crossref] [PubMed]
- Dällenbach P, Kaelin-Gambirasio I, Jacob S, et al. Incidence rate and risk factors for vaginal vault prolapse repair after hysterectomy. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:1623-9. [Crossref] [PubMed]
- Dällenbach P, Kaelin-Gambirasio I, Jacob S, et al. Risk Factors for Pelvic Organ Prolapse Repair After Hysterectomy. Obstet Gynecol 2007;110:625-32. [Crossref] [PubMed]
- DeLancey JO. Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 1992;166:1717-24; discussion 1724-8.
- Elkins T, Hopper J, Goodfellow K, et al. Initial report of anatomic and clinical comparison of the sacrospinous ligament fixation to the high McCall culdoplasty for vaginal cuff fixation at hysterectomy for uterine prolapse. J Pelv Surg 1995;1:12-7.
- Jenkins VR 2nd. Uterosacral ligament fixation for vaginal vault suspension in uterine and vaginal prolapse. Am J Obstet Gynecol 1997;177:1337-43; discussion 1343-4. [Crossref] [PubMed]
- Colombo M, Milani R. Sacrospinous ligament fixation and modified McCall culdoplasty during vaginal hysterectomy for advanced uterovaginal prolapse. Am J Obstet Gynecol 1998;179:13-20. [Crossref] [PubMed]
- Cruikshank SH, Kovac SR. Randomized comparison of three surgical, methods used at the time of vaginal hysterectomy to prevent posterior enterocele. Am J Obstet Gynecol 1999;180:859-65. [Crossref] [PubMed]
- Given FT Jr. “Posterior culdeplasty”: Revisited. Am J Obstet Gynecol 1985;153:135-9. [Crossref] [PubMed]
- Webb MJ, Aronson MP, Ferguson LK, et al. Posthysterectomy vaginal vault prolapse: primary repair in 693 patients. Obstet Gynecol 1998;92:281-5. [PubMed]
- Barber MD, Visco AG, Weidner AC, et al. Bilateral uterosacral ligament vaginal vault suspension with site-specific endopelvic fascia defect repair for treatment of pelvic organ prolapse. Am J Obstet Gynecol 2000;183:1402-10. [Crossref] [PubMed]
- Harris RL, Cundiff GW, Theofrastous JP, et al. The value of intra-operative cystoscopy in urogynecologic and reconstructive pelvic surgery. Am J Obstet Gynecol 1997;177:1367-9. [Crossref] [PubMed]
- Shull BL, Bachofen C, Coates KW, et al. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol 2000;183:1365-73. [Crossref] [PubMed]
- Karram M, Goldwasser S, Kleeman S, et al. High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocele and vaginal vault prolapse. Am J Obstet Gynecol 2001;185:1339-42. [Crossref] [PubMed]
- Amundsen CL, Flynn BJ, Webster GD. Anatomical correction of vaginal vault prolapse by uterosacral ligament fixation in women who also require a pubovaginal sling. J Urol 2003;169:1770-4. [Crossref] [PubMed]
- Tawfeek S, Afifi R. Risk of Ureteral Obstruction with Transvaginal Uterosacral Suspension. J Pelvic Med Surg 2006;12:307-12. [Crossref]
- . AAGL Practice Report: Practice Guidelines on the Prevention of Apical Prolapse at the Time of Benign Hysterectomy AAGL Advancing Minimally Invasive Gynecology Worldwide. J Minimally Invasive Gynecol 2014;21:715-22. [Crossref]
- Craik J, Khan D, Afifi R. The Safety of Intravenous Indigo Carmine to Assess Ureteric Patency During Transvaginal Uterosacral Suspension of the Vaginal Vault. J Pelvic Med Surg 2009;15:11-5. [Crossref]
- McCALL ML. Posterior culdoplasty. Obstet Gynecol 1957;10:595-602.
- Cruikshank SH. Preventing posthysterectomy vaginal vault prolapse and enterocele during vaginal hysterectomy. Am J Obstet Gynecol 1987;156:1433-40. [Crossref] [PubMed]
- Chene G, Tardieu AS, Savary D, et al. Anatomical and functional re- sults of McCall culdoplasty in the prevention of enteroceles and vaginal vault prolapse after vaginal hysterectomy. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:1007-11. [Crossref] [PubMed]
- Alshankiti H, Houlihan S, Robert M. Incidence and contributing factors of perioperative complications in surgical procedures for pelvic organ prolapse. Int Urogynecol J 2019;30:1945-53. [Crossref] [PubMed]
- Gustilo-Ashby AM, Jelovsek JE, Barber MD, et al. The incidence of ureteral obstruction and the value of intra-operative cystoscopy during vaginal surgery for pelvic organ prolapse. Am J Obstet Gynecol 2006;194:1478-85. [Crossref] [PubMed]
- Aronson MP, Aronson PK, Howard AE, et al. Low risk of ureteral obstruction with “deep” (dorsal/posterior) uterosacral ligament suture placement for transvaginal apical suspension. Am J Obstet Gynecol 2005;192:1530-6. [Crossref] [PubMed]
- Buller JL, Thompson JR, Cundiff GW, et al. Uterosacral ligament: description of anatomic relationships to optimise, surgical safety. Obstet Gynecol 2001;97:873-9. [PubMed]
- Gilmour DT, Das S, Flowerdew G. Rates of urinary tract injury from gynecologic surgery and the role of intra-operative cystoscopy. Obstet Gynecol 2006;107:1366-72. [Crossref] [PubMed]
- Jackson E, Bilbao J, Vera R, et al. Risk factors for ureteral occlusion during transvaginal uterosacral ligament suspension. Int Urogynecol J 2015;26:1809-14. [Crossref] [PubMed]
Cite this article as: Sewell T, Tawfeek S, Afifi R. Risk of ureteric injury during ipsilateral uterosacral ligament vault suspension with intra-operative cystoscopy. Gynecol Pelvic Med 2020;3:8.