Laparoscopic uterosacral ligament consolidation and fixation based on the sacrospinous ligament/coccygeus complex
Introduction
Currently, there are three main surgical methods for middle pelvic prolapse, namely sacral colpopexy, sacrospinous ligament fixation (SSLF), and high uterosacral ligament suspension (HUS). Each of the above operations has its own set of complications (1). The complications of sacral colpopexy include intestinal obstruction, ureteral injury, sacral osteitis, thromboembolic symptoms, mesh exposure to the vagina, eroded viscera, ureteral obstruction, etc. The complications of SSLF include rectal injury, compression syndrome of the sciatic nerve, fecal incontinence, etc. The complications of HUS include ureteral injury, ureteral obstruction, etc (2). Most of the complications often require reoperation (Video 1).
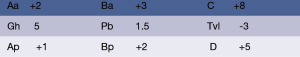
We have completed 50 of these surgeries, with good postoperative recovery and no cases of relapse. This surgery video is of a 68-year-old female patient. She was found to have vaginal prolapse for 20 years with aggravation for 1 year. Her pelvic organ prolapse quantification (POP-Q) score when admitted to the hospital is visible in Figure 1.
Pre-operative assessment
We use the pelvic organ prolapsed quantification method (POP-Q) for staging. Patients with a POP-Q score ≥ II are eligible for the procedure.
Patients are excluded from this procedure if, combined with chronic cough and other medical diseases, they exhibit malignant lesions of the uterus and uterine adnexa.
A preoperative 3D conventional vaginal scrub is performed, and women who have been menopausal for many years and have obvious atrophy of vaginal mucosa are given topical estrogen ointment 1 week before surgery. The patient in the video had an ulcer in the vaginal mucosa, and had to wait for the ulcer to heal before undergoing surgery.
Anaesthesia and positioning
All patients are anesthetized with combined endotracheal intubation and intravenous anesthesia. The umbilical hole is punctured to establish the artificial pneumoperitoneum, the laparoscopic lens with a 10 mm trocar puncture is inserted, and this is followed by insertions of the second trocar in the left abdomen and the third trocar in the right abdomen.
Operative techniques
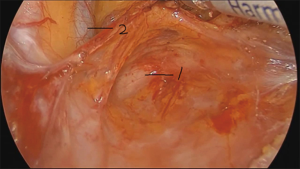
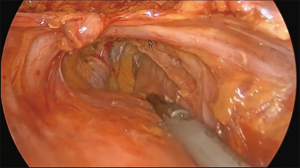
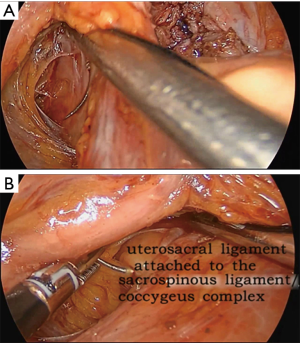
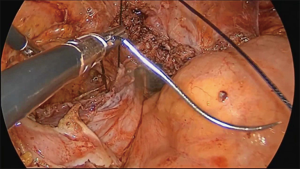
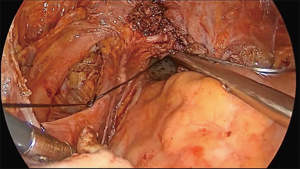
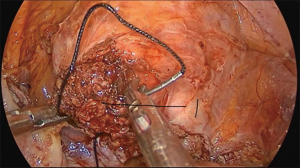
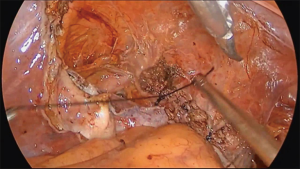
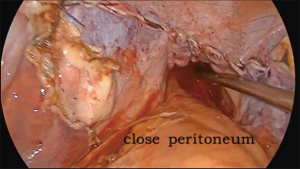
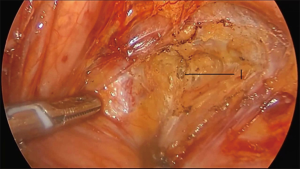
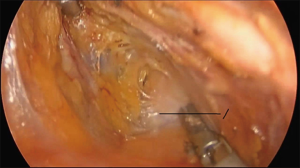
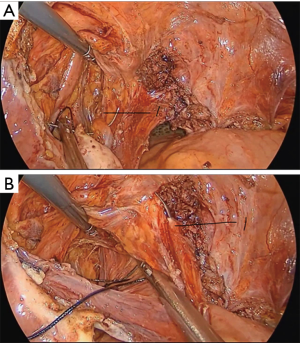
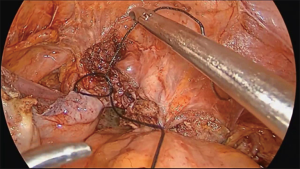
The operation proceeds in the following steps. (I) The position of the ureter is first confirmed. the pelvic peritoneum is cut to the lateral uterosacral ligament by going along the ureter from the pelvic entrance to the ureter 1–2 cm away. The rectal lateral fossa nearby the lateral ureter is sharply separated until the intersection of the ureter and uterine artery. We usually call this the ureteral tunnel (Figure 2). (II) The loose connective tissue of the rectal lateral fossa and the lateral ureter is sharp and blunt separated by ultrasonic knife (Figure 3), and the medial sacrospinous ligament is then exposed. The assistant touches the sciatic spine from the vagina, looking for the sacrospinous ligament. The surgeon gently pulls the sacrospinous ligament with the separation forceps in his left hand to further confirm the sacrospinous ligament. The surgeon use ultrasonic knife to inward and upward separate the medial margin of the sacrospinous ligament, and the sacrospinous ligament/coccygeus complex near the attachment of the sacrum is exposed (Figure 4). (III) An ultrasonic knife is used to cut the lateral serous layer of the uterosacral ligament, push the ureter laterally, and expose the entire lateral section of the uterosacral ligament (Figure 5). (IV) A No. 0 non-absorbable suture with a needle is used to suture the sacrospinous ligament/coccygeus muscle complex near the attachment of the sacrum. The depth of the needle insertion is 3–5 mm (Figure 6A,B). After pulling the suture, in order to make sure there is enough tension (Figure 7), the suture needle is sutured to the sacral part of the uterosacral ligament and then knotted to fix the uterosacral ligament (Figure 8) (first step suture). (V) The lateral edge of the middle part of the uterosacral ligament is then exposed. Next, the stitch which was previously fixed on the sacrospinous ligament/coccygeal complex is used to suture the middle part of the uterosacral ligament with 2–3 stitches (Figure 9A,B). The knot is then tied for the purpose of shortening and strengthening the uterosacral ligament (Figure 10) (second step suture). (VI) The assistant uses oval plier clamps to place a gauze ball into the vagina, raises the vaginal vault and the top of the vagina, and uses the previous non-absorbable suture with a needle to pass through the neck of the uterosacral ligament and the entire top layer of the vagina that has been closed (Figure 11). The mucous membrane or the posterior lateral uterosacral ligament attachment of the cervix should not be penetrated. The suture is tightened, the vaginal tip is pulled 2 cm above the sciatic spine, and the suture is knotted (Figure 12) (third step suture). (VII) These six steps above are also performed on the right side. (VIII) The assistant uses oval plier clamps to place a gauze ball into the vagina again in order to check that the range of motion at the top of the vagina is 1–2 cm. The vagina is then disinfected, and the vaginal stump and the anterior and posterior walls are checked for bulging or bleeding. (IX) Bipolar electrocoagulation is used to stop bleeding during the operation, and the absorption suture is used to close peritoneum (Figure 13).
Postoperative management
According to the routine nursing after laparoscopic surgery, continuous catheter is applied for 5–6 days, with appropriate use of antibiotics. Women who have been menopausal for many years are given topical estrogen. After 5–6 days, the catheter is removed, urine output is observed, and residual urine volume is measured. Regular follow-up is conducted at 1, 3, 6, 9, and 12 months after operation, and a review occurs every 6 months. Medical history is collected (including urine output, presence of prolapse in the vagina or not, or the sensation of prolapse, vaginal examination, POP-Q measurement, residual urine volume, sexual satisfaction, etc.) A subjective cure is defined as patients having no conscious symptoms after surgery, while objective cure is defined as postoperative stage 0 of the top of the vagina or uterus using the POP-Q as the assessment method.
Comments
Uterosacral ligament consolidation and fixation has the following innovations: (I) a change of the fixed position to the sacrospinous ligament/coccygeus complex (physiological attachment point of the uterosacral ligament); (II) making full use of the uterosacral ligament to strengthen the middle section, which solves the problem of uterosacral ligament relaxation lengthening, reduces stress, and conforms more to the concept of self-repair; (III) adopting the “three-step suture technique", which is stable and is not likely to lead to relapse. Firstly, to suture sacrospinous ligament/coccygeus complex with uterosacral ligament for fixation. Secondly, to suture uterosacral ligament with 2–3 stitches for shortening. Lastly, to suture uterosacral ligament with uterus/(top of the vagina) for fixation.
Acknowledgments
The video was awarded the third prize in the First International Elite Gynecologic Surgery Competition (2019 Masters of Gynecologic Surgery).
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Award-Winning Videos from the First International Elite Gynecologic Surgery Competition (2019 Masters of Gynecologic Surgery)”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.org/article/view/10.21037/gpm.2019.12.09/coif). The series “Award-Winning Videos from the First International Elite Gynecologic Surgery Competition (2019 Masters of Gynecologic Surgery)” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Committee on Practice Bulletins-Gynecology, American Urogynecologic Society. Practice Bulletin No. 185: Pelvic Organ Prolapse. Obstet Gynecol 2017;130:e234-e250. [Crossref] [PubMed]
- Subgroup Urogynecology. Chinese Society of Obstetrics and Gynecology, Chinese Medical Association; Urogynecology Subgroup Chinese Society of Obstetrics and Gynecology Chinese Medical Association. Guideline for the diagnosis and management of pelvic organ prolapse (draft). Zhonghua Fu Chan Ke Za Zhi 2014;49:647-51.
Cite this article as: Huang W, Chen C, Yang Z, Lan X, Fang Z. Laparoscopic uterosacral ligament consolidation and fixation based on the sacrospinous ligament/coccygeus complex. Gynecol Pelvic Med 2020;3:6.