Laparoendoscopic single site surgery for severe pelvic adhesion release and total hysterectomy with bilateral salpingectomy
Highlight box
Key findings
• Severe pelvic adhesion release and total hysterectomy with bilateral salpingectomy could be performed with laparoendoscopic single site surgery (LESS).
What is conventional and what is novel/modified?
• LESS can be used for total hysterectomy, but due to difficulties in visual field exposure and instrument interference, it is challenging to operate in cases of severe pelvic adhesion.
• We provided a surgical video that demonstrated the successful completion of a total hysterectomy using LESS despite severe pelvic adhesions.
What is the implication, and what should change now?
• Gynecologists must be well-acquainted with the advantages and disadvantages of the visual field and operation of single-port laparoscopy, as well as the strengths and weaknesses of various laparoscopic instruments, in order to safely perform various complex surgeries.
Introduction
In worldwide, hysterectomy is one of the most common gynecological procedure (1). For many years, this procedure was performed via open surgery or vaginally. To achieve a minimally invasive surgery, laparoscopic hysterectomy is developed. The advantages of laparoscopic surgery are smaller surgical wounds, less pain, shorter hospital stay, and fewer complications (2). The umbilicus is a natural orifice and the scar on it is hided by folds of skin. Laparoendoscopic single-site surgery (LESS) is a new type of laparoscopic surgery, which is performed through a 2–3 cm incision in the umbilicus, and the laparoscope and instruments are inserted to complete the operation (3). Pelosi et al. in 1991 reported the first LESS hysterectomy (4). Compared with the traditional surgery, LESS has less trauma, better cosmetic effect and higher patients’ satisfaction. At our hospital, since the introduction of LESS in 2017, LESS hysterectomy gradually became the main management for symptomatic adenomyosis or uterine fibroids. However, gynecologists may convert LESS to multiport laparoscopy or laparotomy for bleeding control or severe pelvic adhesion. This video aims to describe a case for severe pelvic adhesion release and total hysterectomy with bilateral salpingectomy. We present this article in accordance with the SUPER reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-24-28/rc).
Preoperative preparations and requirements
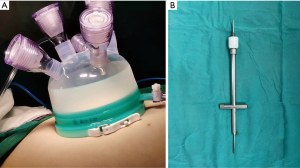
To perform the procedure, we utilized a single-port access platform (Figure 1A), a uterine manipulator (Figure 1B), a 10-mm 30-degree standard-length optical camera, ultrasonic knife, bipolar electrocautery, prototype of laparoscopic instruments. The patient was set in the lithotomy position. All procedures were performed under general anesthesia. We placed the uterine manipulation into the cervix from the vagina and a urinary catheter was inserted. The chief surgeon stood on the left side of the patient and the first assistant stood on the other side, while the second assistant, handling the uterine manipulator, sat between legs. CO2 was injected into the abdominal cavity, and the pneumoperitoneum pressure was maintained at
14 mmHg.
All procedures performed in this study were in accordance with the Helsinki Declaration (as revised in 2013). This study was approved by the ethics committee on human research at West China Second Hospital, Sichuan University (No. 2023139). The patient provided informed consent for the publication of her clinical and imaging data.
Step-by-step description
Video 1 demonstrates step-by-step on how to perform LESS for severe pelvic adhesion release and total hysterectomy with bilateral salpingectomy.
- Step 1: releasing adhesion between the uterus and sigmoid colon.
- Step 2: cauterization of utero-ovarian ligaments and tube pedicles.
- Step 3: cauterization and transection of the round ligament.
- Step 4: dissection of anterior broad ligament peritoneum.
- Step 5: dissection of the bladder.
- Step 6: dissection of uterosacral ligaments.
- Step 7: dissection and cutting of the uterine vessels.
- Step 8: opening of the vaginal walls and removal of the uterus.
- Step 9: suture of vaginal walls.
- Step 10: controlling bleeding before removal of the laparoscope and the port.
Postoperative considerations and tasks
A 49-year-old female with symptomatic adenomyosis and uterine fibroid was performed LESS hysterectomy with bilateral salpingectomy. The uterus weight was 570 g, surgical duration was 146 minutes and estimated blood loss was 110 mL. After the patient recovered from anesthesia for 6 hours, she started liquid diet. The urinary catheter was removed on the second postoperative day and the patient was discharged on the third day. We followed the patient at 2 weeks and 2 months to visualize the suture of the vaginal walls. There was no morbidity.
Tips and pearls
Before surgery, gynecologists should fully communicate the patient’s condition and surgical risks with the patient and her family. The patient should be fully informed and understand that the available surgical option is laparotomy, multi-port laparoscopy, or LESS. The CO2 pneumoperitoneum should be closed to prevent intra-abdominal blood or wash from splashing onto the assistant through the vagina, when we removed the uterus. The most important thing is to protect the ureters during surgery, avoiding direct mechanical injury or thermal radiation damage from energy devices.
Discussion
There are several advantages of LESS, such as better cosmetic outcomes, less hospital stay (5,6). However, the disadvantage of LESS must be noticed, that is, “chopstick effect”. The “chopstick effect” caused by the interference of instruments, which made delicate operations such as separating intestinal adhesions challenging (7). Besides, LESS may convert to multiple port laparoscopy or laparotomy due to pelvic adhesions or bleeding (8).
In our work, this surgery was a case of LESS severe pelvic adhesion release and total hysterectomy with bilateral salpingectomy. After the laparoscope was inserted, dense adhesions between the sigmoid colon and the uterus were discovered, necessitating the separation of intestinal adhesions to perform the hysterectomy. The surgeon had mastered the operation of LESS, and this video demonstrated the surgeon’s skilled use of an ultrasonic knife and scissors for the delicate operation of separating intestinal adhesions, minimizing intestinal damage while exposing the surgical field. After the adhesions were separated and the pelvis was fully exposed, the total hysterectomy with bilateral salpingectomy could proceed smoothly. This suggested that after a myomectomy, the use of anti-adhesion materials could be considered to reduce the occurrence of pelvic adhesions.
Regarding surgical complications, several studies have found that compared to multi-port laparoscopy, LESS does not increase perioperative complications, postoperative pain, or conversion to open surgery, and it does not extend hospital stay, with only a slight increase in surgical time (13 minutes) (5,6). However, in patients with a history of cesarean section, the risk of urinary system injury is higher (9). In LESS procedures, injuries to the bladder or ureter may occur due to instrument interference, insufficient visualization, or thermal effects from energy devices, which requires particular attention from the surgeon.
In our work, vaginal suturing is performed laparoscopically because this approach allows gynecologists to better expose the anterior and posterior vaginal walls, even by suspending the bladder, resulting in better suturing outcomes. Previous publications also show that for vaginal suture, laparoscopy is a safe and less time-consuming procedure (10,11).
Conclusions
For symptomatic adenomyosis and uterine fibroid, which is ineffective to medicine treatment, hysterectomy with bilateral salpingectomy is the effective therapy. For the requirement of rapid recovery, LESS hysterectomy may be a better choice. However, “chopstick effect” becomes the greatest difficulty of LESS and gynecologists need more practice. These surgical skills may overcome the difficulties and defects of LESS, and could make the operation more convenient. LESS technique is a feasible and safe approach for severe pelvic adhesion release and hysterectomy with bilateral salpingectomy.
Acknowledgments
The video in this study was awarded the third prize in the Fourth International Elite Gynecologic Surgery Competition (2024 Masters of Gynecologic Surgery).
Funding: This work was supported by
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Gynecology and Pelvic Medicine for the series “Award-Winning Videos from the Fourth International Elite Gynecologic Surgery Competition (2024 Masters of Gynecologic Surgery)”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-24-28/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-24-28/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-24-28/coif). The series “Award-Winning Videos from the Fourth International Elite Gynecologic Surgery Competition (2024 Masters of Gynecologic Surgery)” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the Helsinki Declaration (as revised in 2013). This study was approved by the ethics committee on human research at West China Second Hospital, Sichuan University (No. 2023139). The patient provided informed consent for the publication of her clinical and imaging data.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nieboer TE, Johnson N, Lethaby A, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 2009;CD003677. [PubMed]
- Reich H. Total laparoscopic hysterectomy: indications, techniques and outcomes. Curr Opin Obstet Gynecol 2007;19:337-44. [Crossref] [PubMed]
- Boruta DM. Laparoendoscopic single-site surgery in gynecologic oncology: An update. Gynecol Oncol 2016;141:616-23. [Crossref] [PubMed]
- Pelosi MA, Pelosi MA 3rd. Laparoscopic hysterectomy with bilateral salpingo-oophorectomy using a single umbilical puncture. N J Med 1991;88:721-6. [PubMed]
- Jo EJ, Kim TJ, Lee YY, et al. Laparoendoscopic single-site surgery with hysterectomy in patients with prior cesarean section: comparison of surgical outcomes with bladder dissection techniques. J Minim Invasive Gynecol 2013;20:160-5. [Crossref] [PubMed]
- Xie W, Cao D, Yang J, et al. Single-Port vs Multiport Laparoscopic Hysterectomy: A Meta-Analysis of Randomized Controlled Trials. J Minim Invasive Gynecol 2016;23:1049-56. [Crossref] [PubMed]
- Dou Y, Wang Y, Tang S, et al. Learning curve for laparoendoscopic single-site radical hysterectomy using the "chopstick" technique: a retrospective cohort study. Ann Transl Med 2022;10:1165. [Crossref] [PubMed]
- Song T, Lee Y, Kim ML, et al. Single-port access total laparoscopic hysterectomy for large uterus. Gynecol Obstet Invest 2013;75:16-20. [Crossref] [PubMed]
- Rattanakanokchai S, Kietpeerakool C, Srisomboon J, et al. Perioperative Complications of Hysterectomy After a Previous Cesarean Section: A Systematic Review and Meta-Analysis. Clin Epidemiol 2019;11:1089-98. [Crossref] [PubMed]
- Uccella S, Malzoni M, Cromi A, et al. Laparoscopic vs transvaginal cuff closure after total laparoscopic hysterectomy: a randomized trial by the Italian Society of Gynecologic Endoscopy. Am J Obstet Gynecol 2018;218:500.e1-500.e13. [Crossref] [PubMed]
- Bastu E, Yasa C, Dural O, et al. Comparison of 2 Methods of Vaginal Cuff Closure at Laparoscopic Hysterectomy and Their Effect on Female Sexual Function and Vaginal Length: A Randomized Clinical Study. J Minim Invasive Gynecol 2016;23:986-93. [Crossref] [PubMed]
Cite this article as: Zhao J, Liao S, Min L. Laparoendoscopic single site surgery for severe pelvic adhesion release and total hysterectomy with bilateral salpingectomy. Gynecol Pelvic Med 2024;7:35.