
Uterine tumor with characteristics of ovarian sex-cord tumor: case report
Highlight box
Key findings
• This case report describes a rare uterine tumor with characteristics of ovarian sex-cord tumor and aims to provide a better understanding of the clinical features and surgical indications of uterine tumor similar to ovarian sex cord tumor (UTROSCT).
What is known and what is new?
• UTROSCT represents less than 1% of uterine mesenchymal tumors. Despite generally not exhibiting malignant behavior, it presents symptoms that impact the quality of life of patients.
• We present a video-hysterectomy converted to laparotomy due to bladder injury, as UTROSCT has surgical indications to prevent complications.
What is the implication, and what should change now?
• The rarity of this case contributes to the understanding of the literature regarding the diagnosis, management, and treatment of UTROSCT.
Introduction
Uterine tumor that presents similar characteristics to ovarian sex cord tumors is a rare form of uterine neoplasia that was initially reported by Morehead and Bowman in 1945 (1), after the uterine tumor similar to ovarian sex cord tumor (UTROSCT) was classified in 1976 by Scully and Clement (2). This condition most commonly affects postmenopausal women, typically occurring between the fourth and sixth decades of life (2). The tumor causes clinical consequences similar to those of other diseases of the female reproductive system, therefore, it is a complex diagnosis made exclusively by histopathological analysis (3). The main biological markers employed for diagnosis include WT-1, calretinin and inhibin, along with smooth muscle markers such as h-caldesmon, desmin and smooth muscle actin. Epithelial tissue markers such as cytokeratin AE1 and AE3, as well as CD10, CD99, and melan-A, are also used (3).
Among the possible differential diagnosis of uterine malignancies are endometrial connective tissue sarcomas, which the World Health Organization classifies into four distinct groups: endometrial stromal nodule, low-grade endometrial stromal sarcoma (LG-ESS), high-grade ESS (HG-ESS) and undifferentiated uterine sarcoma (4). These endometrial stromal neoplasms generally present with symptoms such as uterine mass, abnormal uterine bleeding and pelvic pain, similar to those of UTROSCT, although it has a worse prognosis.
The diagnosis of these conditions is also often made after performing a hysterectomy or myomectomy, originally scheduled to treat presumed benign leiomyomas (5). Therefore, it is necessary to differentiate UTROSCT, this and other neoplasms, through anatomopathological and immunohistochemical analysis, so that the conduct is appropriate.
Despite the current biologically benign trajectory of this tumor, there are controversies regarding its progression. There are some indications of risk factors for recurrence and metastasis, such as advanced age, presence of necrosis, lymphovascular invasion, cervical involvement, nuclear atypia and increased mitotic activity (6). For this reason, most cases will require surgical procedures. The extent of surgery is based on the aggressiveness of the tumor and, for cases of substantial risk, radical procedures such as hysterectomy, salpingectomy, parametrial resection, pelvic and para-aortic lymphadenectomy are considered (7). However, before surgical interventions, the patient’s family planning must be considered.
In this report, we detail a case involving a uterine tumor similar to an ovarian sex cord tumor. We discuss its clinical and histopathological characteristics, treatment and evolution in a patient with active menstrual cycles. The patient presented a uterine mass and enlarged uterus, which required surgical intervention. We present this article in accordance with the CARE reporting checklist (available at https://gpm.amegroups.com/article/view/10.21037/gpm-24-11/rc).
Case presentation
The patient is a 48-year-old woman, whose menarche occurred at the age of 12 years old and the onset of sexual activity began at the age of 21 years old. She used contraceptive pills for 21 years (resulting in menstruation lasting between three and four days), with interruptions due to periods of pregnancy (four pregnancies: two miscarriages and two cesarean deliveries). She has a history of systemic arterial hypertension, previous surgeries to remove the gallbladder by laparoscopy, two cesarean deliveries—a uterine opening procedure with a Pfannenstiel-type skin incision—and orthopedic surgery associated with 1 exploratory laparotomy with a median skin incision in the linea alba to treat a fracture of the hip bones induced by a car accident and uterine hemorrhagic injury due to fractured bone structures.
In the medical history, the patient sought a gynecological consultation in 2021 due to heavy menstrual flow (lasting between 12 and 15 days of bleeding) and pelvic pain. Pelvic and transvaginal ultrasounds were performed, which revealed a single mass measuring 3.22 cm × 2.54 cm with heterogeneous echogenicity in which multiple anechoic areas with central and peripheral vascularization were present on power doppler diagnosed as a uterine fibroid and a slight increase in uterine volume. After six months, the patient returned to the office and underwent a new ultrasound (Figure 1), which revealed the presence of two additional leiomyomatous lesions measuring 50.99 mm × 46.72 mm and 26.48 mm × 20.21 mm respectively presenting heterogeneous echogenicity in which multiple anechoic areas with central and peripheral vascularization were present on power doppler. As a result, the doctor recommended a total hysterectomy and bilateral salpingectomy.

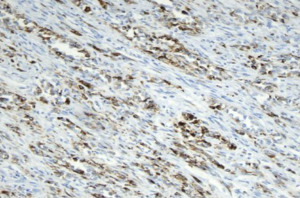
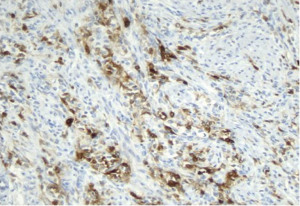
The surgery was performed by two surgeons (a gynecologist and a gynecological oncologist). The initial procedure was a laparoscopic hysterectomy and removal of the adnexa. However, due to numerous adhesions resulting from previous surgeries in the abdominopelvic cavity, complications arose, resulting in an apical bladder injury of approximately 2 cm, which occurred when trying to separate the visceral peritoneum that covered both organs. Consequently, the surgery was converted into a laparotomy with a Pfannenstiel-type incision to perform cystorrhaphy and remove the uterus, which occurred without other complications. After the surgical intervention that took place in 2022, the collected tissue was sent to the histopathological laboratory, which identified two leiomyomatous lesions and a neoplastic lesion called a uterine tumor with characteristics similar to an ovarian sex cord tumor (lesions for which markers were exemplified in Figures 2,3). At a macroscopic exam of the lesion, the uterus surface present changed due the presence of a single, yellowish, and well-defined mass with soft and fibrous aspect measuring 50 mm in the largest axis. The histological exam presents lesions described by infiltration with a diffuse, chordal and microtubule arrangement, composed of small to medium-sized cells with ovoid nuclei, a histological pattern similar to ovarian sex cord tumors. The definitive diagnosis was made by the immunohistochemical analysis which showed: estrogen receptor (+), CD10 (+), WT1(+), calretinin (+), AE1/AE3 (+), 1A4 (+), FOXL2 (−), inhibin (−), desmin (−), melan-A (−) EMA (−). Serum tumor markers such as CD10 and TW1 were searched due to their importance in evaluating the cancer progression (8,9). The immunohistochemistry slide presented in Figure 2 shows cytokeratins markers, proteins responsible for the formation of intermediate filaments in epithelial cells. The markers AE1 and AE3 are monoclonal antibodies that recognize cytokeratins and are used to diagnose and classify benign and malignant tumors. They also allow for the identification of epithelial cells in histological samples, differentiating carcinomas from other tumor types. The Figure 3 shows an immunohistochemistry slide with the presence of calretinin, a protein that plays an important role in modulating neuronal excitability and regulating intracellular calcium, as well as being an important marker for various diseases. Both slides were produced using a 40× objective lens and a 10× eyepiece, resulting in a total magnification of 400×.
After surgery, the patient was referred to the oncology service for further investigation and examinations during a month. Blood markers yielded negative results for any metastatic neoplasm, and the abdominal and pelvic magnetic resonance imaging (MRI) was normal, confirming this finding. Consequently, as the tests did not indicate the persistence of the cancer, she was discharged from the oncology service and was referred back to the gynecologist’s office for regular follow-up during the next years with no further complaints arising from the patient.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was not obtained from the patient or the relatives after all possible attempts were made. The article has been sufficiently anonymized to cause no harm to the patient or her family.
Discussion
Uterine tumors that resemble ovarian sex cord tumors macroscopically resemble a uterine fibroid. Microscopic investigation presents several receptors that are characterized as uterine neoplasia due to genetic mutations and reduction or absence of factors regulating the mitotic cycle, but with benign evolution (2), however, some authorities have proposed that UTROSCT be classified as a potentially malignant tumor indeterminate due to recurrences of lymphatic metastases or postoperative recurrences.
The diagnosis of this type of tumor is histopathological, as clinical signs are ineffective. The clinical characteristics of the tumor are long-lasting metrorrhagia, pelvic pain and ultrasound results showing leiomyomatous lesions with a significant increase in uterine volume. This set of symptoms is common to several benign and malignant gynecological pathologies (2).
Macroscopically, the tumor is a single, well-defined lesion, yellowish in color and located intramurally. Histology shows lesions described by infiltration with a diffuse, chordal and microtubule arrangement, composed of small to medium-sized cells with ovoid nuclei, a histological pattern similar to ovarian sex cord tumors (2).
The patient’s immunohistochemical examination showed estrogen receptor (+), CD10 (+), WT1 (+), calretinin (+), AE1/AE3 (+), 1A4 (+), FOXL2 (−), inhibin (−), desmin (−), melan-A (−) EMA (−). The immunohistochemistry slide presented in Figure 2 shows cytokeratins markers, proteins responsible for the formation of intermediate filaments in epithelial cells. The markers AE1 e AE3 are monoclonal antibodies that recognize cytokeratins and are used to diagnose and classify benign and malignant tumors. They also allow for the identification of epithelial cells in histological samples, differentiating carcinomas from other tumor types. Figure 3 shows an immunohistochemistry slide with the presence of calretinin, a protein that plays an important role in modulating neuronal excitability and regulating intracellular calcium, as well as being an important marker for various diseases. Both slides were produced using a 40× objective lens and a 10× eyepiece, resulting in a total magnification of 400×. Furthermore, serum tumor markers such as CD10 and TW1, indicate cancer progression and prognosis.
The presence of receptors for ovarian sex hormones increases the possibility of the neoplasm originating from elements of the ovarian sex cords; the presence of receptors for muscle trophic factors (desmin, actin) indicates that the origin may be epithelial or muscular. These sex cord elements may originate from ectopic ovarian tissue in the uterine wall or from uterine stromal cells with divergent differentiation capabilities (10), but pathologists do not yet have a complete understanding of their histopathological features.
Regarding treatment, the best option for this patient, a 48-year-old woman with two teenage children, is to perform a total hysterectomy and bilateral salpingectomy in a single surgical approach, this way the lesion is completely removed and recurrences are avoided. However, the possibility of preserving fertility should be discussed with patients, taking into account their reproductive planning, but informing them of the risks (5). In the report described, total hysterectomy was chosen because the patient, 48 years old, with 2 children, had complete planning.
For surgery, a laparoscopy was initiated, due to its indications of better results, such as reduced blood loss, shorter hospital stays and less need for postoperative analgesics (11). However, due to peritoneal adhesions, hysterectomy required conversion to laparotomy.
The patient’s evolution after this approach was benign and his general health status improved considerably, bringing the benefits of surgical intervention for the treatment of UTROSCT, although this study is still limited by the short observation time. In addition, there is continuous medical monitoring with oncology and gynecology for investigation and patient care (7).
Conclusions
UTROSCT is a rare condition, accounting for less than 1% of uterine mesenchymal tumors (12). The UTROSCT was first reported by Morehead and Bowman in 1945 (1). After, in 1976, Clement and Scully classified the lesions into two subgroups. This type of tumor still presents uncertainties regarding its origin, patterns and evolution (2). Although the neoplasm generally presents a favorable prognosis, there are reports of cases with extrauterine metastases and deaths resulting from this type of tumor in patients who did not undergo surgical intervention or only isolated hysterectomy (6). In contrast, extended radical surgery can drastically reduce the recurrence rate, even in aggressive cases. There is, therefore, in patients who have smaller tumors and which do not compromise uterine physiology, the possibility of, during surgery, simply removing the mass so that the patient’s fertility is preserved. This technique is used in young patients who want to have children, but it is a risk given the possibility of the neoplasia returning. Therefore, correct assessment and application of the appropriate technique are necessary for successful treatment.
Furthermore, the diagnosis of uterine tumor with features of ovarian sex cord tumor is challenging. The rarity of the neoplasm means that it is only discovered after analyzing postoperative samples in which other pathologies were suspected. As a consequence, diagnosis is often late, which can make treatment more complex and lead to inadequate or insufficient surgical interventions (7). Likewise, the disease has a diverse immunohistochemical profile that can be confused with tumors from other tissues, which also makes its identification challenging (13).
All these factors, and the rarity of UTROSCT, mean that it is often only discovered after analyzing postoperative samples in which other pathologies were suspected, as in the case described. Therefore, it is necessary for the medical team to always be aware of the possibility that it is a malignant tumor, applying measurable preoperative schemes to improve the standardization of the diagnosis of uterine fibroids identified on imaging and other methods, using, for example, Myoma Score. In this way, it is possible to classify patients as having low or high risk of malignancy in advance, so that appropriate precautions can be taken during the surgical procedure (14).
Finally, the report presented contributes to greater dissemination of this type of tumor, so that knowledge about the existence of the neoplasm facilitates its diagnosis, improving the management of the disease and achieving better results. Furthermore, as this is a rare case that still requires clarification, it is recommended that patients with uterine tumors with characteristics of an ovarian sex cord tumor remain under medical supervision to monitor possible complications and recurrences.
Patient perspective
Since the initiation of the diagnosis of myomatous lesion, the patient had displayed concerns regarding her treatment, primarily due to her medical history and her anemic state resulting from heavy menstrual flow. However, even subsequent to the confirmation of UTROSCT, the patient, despite harboring apprehensions towards the diagnosis, reported that the medical support she received aided her in managing the condition and alleviating her worries.
Furthermore, the patient conveyed having well-received the proposed treatment, exhibiting trust in the professionals who aided her and expressing satisfaction with the postoperative period.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://gpm.amegroups.com/article/view/10.21037/gpm-24-11/rc
Peer Review File: Available at https://gpm.amegroups.com/article/view/10.21037/gpm-24-11/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gpm.amegroups.com/article/view/10.21037/gpm-24-11/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent for publication of this case report and accompanying images was not obtained from the patient or the relatives after all possible attempts were made. The article has been sufficiently anonymized to cause no harm to the patient or her families.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Morehead RP, Bowman MC. Heterologous Mesodermal Tumors of the Uterus: Report of a Neoplasm Resembling a Granulosa Cell Tumor. Am J Pathol 1945;21:53-61. [PubMed]
- Clement PB, Scully RE. Uterine tumors resembling ovarian sex-cord tumors. A clinicopathologic analysis of fourteen cases. Am J Clin Pathol 1976;66:512-25. [Crossref] [PubMed]
- Czernobilsky B. Uterine tumors resembling ovarian sex cord tumors: an update. Int J Gynecol Pathol 2008;27:229-35. [Crossref] [PubMed]
- Hanby A, Walker C, Tavassoli FA, Devilee P. Pathology and Genetics: Tumours of the Breast and Female Genital Organs. WHO Classification of Tumours series - volume IV. Lyon, France: IARC Press. Breast Cancer Res 2004;6:133. [Crossref]
- Giannini A, Golia D'Augè T, Bogani G, et al. Uterine sarcomas: A critical review of the literature. Eur J Obstet Gynecol Reprod Biol 2023;287:166-70. [Crossref] [PubMed]
- Moore M, McCluggage WG. Uterine tumour resembling ovarian sex cord tumour: first report of a large series with follow-up. Histopathology 2017;71:751-9. [Crossref] [PubMed]
- Sato M, Yano M, Sato S, et al. Uterine tumor resembling ovarian sex-cord tumor (UTROSCT) with sarcomatous features without recurrence after extended radical surgery: A case report. Medicine (Baltimore) 2020;99:e19166. [Crossref] [PubMed]
- Mishra D, Singh S, Narayan G. Role of B Cell Development Marker CD10 in Cancer Progression and Prognosis. Mol Biol Int 2016;2016:4328697. [Crossref] [PubMed]
- Sugiyama H. WT1 (Wilms' tumor gene 1): biology and cancer immunotherapy. Jpn J Clin Oncol 2010;40:377-87. [Crossref] [PubMed]
- Lillemoe TJ, Perrone T, Norris HJ, et al. Myogenous phenotype of epithelial-like areas in endometrial stromal sarcomas. Arch Pathol Lab Med 1991;115:215-9. [PubMed]
- Giannini A, Cuccu I, D'Auge TG, et al. The great debate: Surgical outcomes of laparoscopic versus laparotomic myomectomy. A meta-analysis to critically evaluate current evidence and look over the horizon. Eur J Obstet Gynecol Reprod Biol 2024;297:50-8. [Crossref] [PubMed]
- Höhn AK, Brambs CE, Hiller GGR, et al. 2020 WHO Classification of Female Genital Tumors. Geburtshilfe Frauenheilkd 2021;81:1145-53. [Crossref] [PubMed]
- Zhang X, Zou S, Gao B, et al. Uterine tumor resembling ovarian sex cord tumor: a clinicopathological and immunohistochemical analysis of two cases and a literature review. J Int Med Res 2019;47:1339-47. [Crossref] [PubMed]
- Wojdat R, Malanowska E. An evaluation of a Myomscore in the preoperative assessment of uterus myomatosus: a new diagnostic standard? The experience at the Mathilden Hospital in Herford, Germany. Gynecol Surg 2020;17:9. [Crossref]
Cite this article as: de Oliveira NM, de Oliveira MC, Correa BM, de Faria IM. Uterine tumor with characteristics of ovarian sex-cord tumor: case report. Gynecol Pelvic Med 2024;7:28.


